Theophylline Dose Adjustment Calculator
Theophylline Safety Calculator
This calculator helps determine the appropriate theophylline dose adjustment when interacting medications are taken or when clearance changes (e.g., smoking cessation). Theophylline has a narrow therapeutic range (10-20 mcg/mL) and toxicity risk increases dramatically when clearance decreases.
Current Medication Status
Results
Please enter your current dose and select any interacting medications to see results.
Theophylline isn’t used as often as it used to be, but for some people - especially those with severe asthma or COPD who don’t respond to newer inhalers - it’s still a lifeline. The problem? It’s a narrow-margin drug. That means the difference between helping and harming is small. And one of the biggest dangers isn’t taking too much, it’s taking the same dose while your body suddenly can’t clear it anymore. This happens when other medications you’re on slow down how fast your liver breaks down theophylline. The result? Toxic levels build up. You might not feel it at first. Then comes nausea, a racing heart, seizures, or worse.
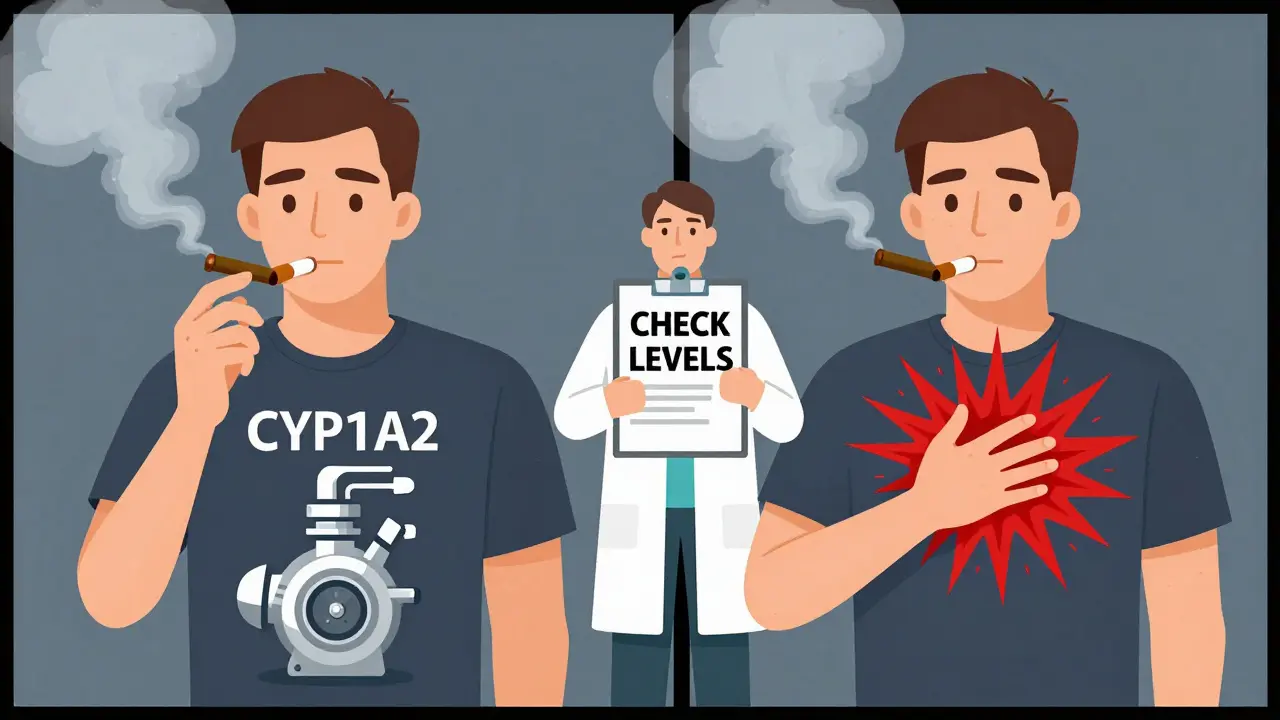
Why theophylline clearance matters so much
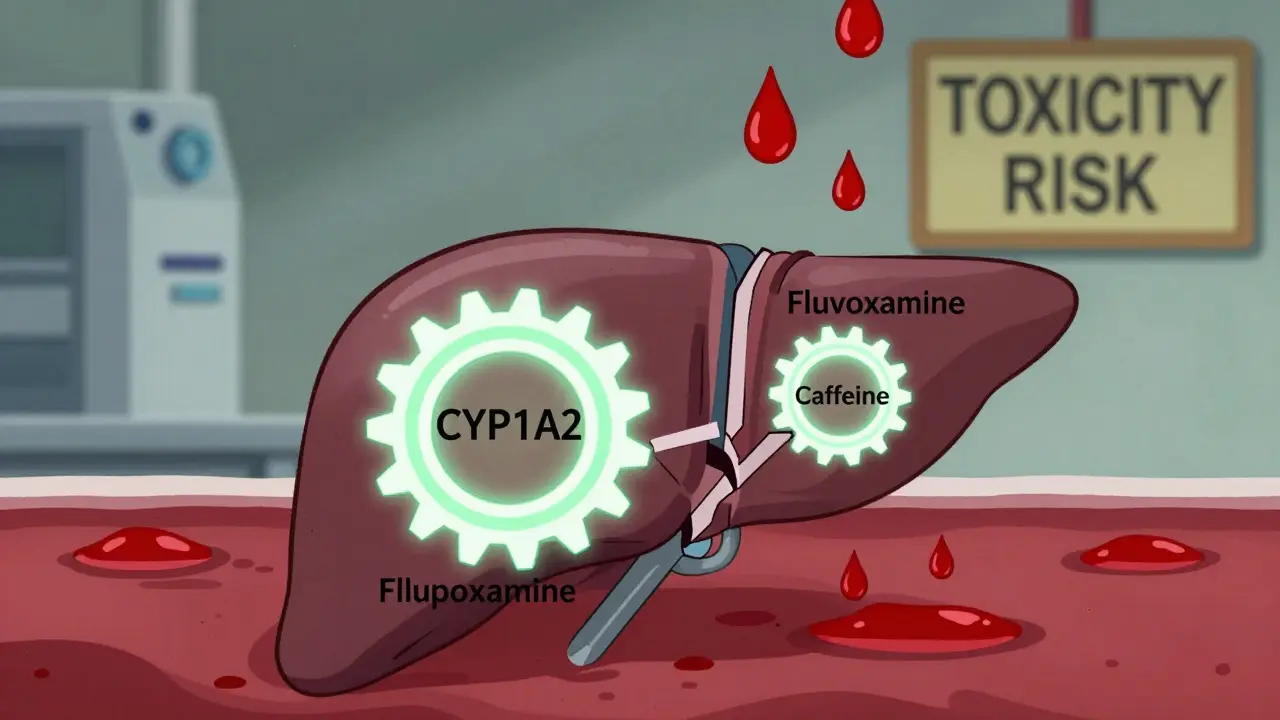
Theophylline is cleared mostly by your liver, using a specific enzyme called CYP1A2. About 90% of it gets broken down this way. The rest leaves your body unchanged through urine. This enzyme doesn’t just handle theophylline - it processes caffeine, some antidepressants, and even some painkillers. That’s why interactions are so common.Normal clearance in a healthy adult is around 3 liters per hour. But if you’re older, have heart failure, or don’t smoke, that number drops. Smokers clear it faster - sometimes up to 3 times faster - because smoking boosts CYP1A2 activity. When you quit smoking, clearance plummets by 30-50% within weeks. That alone can push levels into the toxic range. Add a medication that blocks CYP1A2, and you’re playing with fire.
The therapeutic range? 10 to 20 micrograms per milliliter. Go above 20, and side effects become likely. Above 30? That’s medical emergency territory. And because theophylline follows non-linear kinetics, a small drop in clearance doesn’t just slightly raise levels - it can cause a massive, unpredictable spike. A 20% reduction in metabolism might push your level from 15 to 28. No dose change. No warning. Just toxicity.
Medications that dangerously slow theophylline clearance
Not all drugs affect theophylline the same way. Some barely move the needle. Others are outright dangerous. Here are the big ones, backed by clinical data:- Fluvoxamine - This SSRI antidepressant is one of the strongest CYP1A2 inhibitors out there. Studies show it cuts theophylline clearance by 40-50%. The European Respiratory Society says to avoid combining them entirely. If you’re on fluvoxamine and theophylline, your doctor should have switched you to something else already.
- Cimetidine - This old-school heartburn pill (Tagamet) is still prescribed. It reduces theophylline clearance by 25-30%. In one hospital study, cimetidine was involved in nearly 30% of theophylline toxicity cases. A patient on stable theophylline might start cimetidine for acid reflux, and within 72 hours, their serum level jumps from 15 to 25. They end up in the ER with vomiting and palpitations.
- Allopurinol - Used for gout, this drug cuts clearance by about 20%. It’s not as dramatic as fluvoxamine, but it’s sneaky. Many doctors don’t realize it matters. A 2023 survey found 15% of theophylline toxicity cases involved allopurinol. The fix? Reduce theophylline by 20% when starting allopurinol.
- Erythromycin and clarithromycin - These antibiotics are often given for lung infections. They don’t directly block CYP1A2, but they inhibit CYP3A4, which plays a supporting role. Clearance drops 15-25%. If you’re on theophylline and get pneumonia, your doctor needs to know - and adjust your dose before you even leave the clinic.
These aren’t theoretical risks. In a 2021 study of over 1,200 older patients on theophylline, nearly 30% were also taking at least one of these drugs - and only 37% had their dose adjusted. That’s a recipe for disaster.

What about other common drugs?
Not everything slows clearance. Some drugs do the opposite.- Phenytoin, phenobarbital, rifampicin - These drugs increase theophylline clearance by 30-60%. If you’re on one of these, your theophylline level might drop below therapeutic range. You’ll feel your asthma getting worse. Your doctor needs to increase your dose.
- Furosemide - The evidence is mixed. Some studies say it cuts clearance by 10-15%. Others say no effect. If you’re on both, monitor closely - but don’t assume it’s a major problem.
And don’t forget lifestyle. Smoking cessation? That’s a big one. If you quit smoking while on theophylline, your clearance drops fast. You might need a 30% dose reduction. No one tells you that. That’s why so many patients end up in the hospital after quitting.
Real-world impact: What happens when this goes wrong
The FDA says roughly 2,000 emergency visits each year in the U.S. are due to theophylline toxicity - and 35% of those are from drug interactions. In a 2022 report from the American College of Chest Physicians, 63% of hospitalized cases involved CYP1A2 inhibitors. Cimetidine, fluvoxamine, and allopurinol were the top three.Here’s a real case from a community pharmacy log: A 72-year-old woman with COPD had been on 400 mg of theophylline daily for 5 years. Her level was stable at 15.2 mcg/mL. She started cimetidine for GERD. Three days later, she was vomiting, dizzy, and her heart was fluttering. Her new level? 24.7 mcg/mL. She was admitted. She didn’t have a heart condition. She didn’t overdose. She just took two common drugs that didn’t play nice.
Surveys show 78% of pulmonologists have seen at least one serious interaction in the past year. Yet 62% say their electronic health records don’t warn them properly. Pharmacists often catch it first - because they see the full list. But if the prescriber doesn’t know, the patient pays the price.
How to stay safe
If you’re on theophylline, here’s what you need to do:- Always tell your doctor every medication you take - even over-the-counter ones. Many people don’t think antacids or sleep aids count.
- Ask if any new drug you’re prescribed affects CYP1A2. If you’re unsure, ask: “Does this interact with theophylline?”
- Get your blood level checked within 48-72 hours after starting or stopping any new medication. Don’t wait for symptoms.
- Don’t quit smoking cold turkey without talking to your doctor. Your dose may need to come down.
- Know the warning signs: Nausea, vomiting, rapid heartbeat, tremors, confusion. If you feel this way, go to urgent care - don’t wait.
Some guidelines, like NICE in the UK, recommend avoiding theophylline entirely if you need long-term cimetidine or fluvoxamine. There’s no point risking toxicity when better alternatives exist. But in places where newer drugs are expensive or unavailable, theophylline remains essential. That’s why managing interactions isn’t optional - it’s life-saving.
What’s changing?
The use of theophylline is falling. In the U.S., it’s down 62% since 2000. But in parts of Asia and Africa, it’s still common. That means more people are at risk - and fewer doctors are trained to spot the interactions.There’s new interest in very low-dose theophylline (100-200 mg) for its anti-inflammatory effects in COPD. But trials now explicitly exclude people on CYP1A2 inhibitors. That tells you how serious the risk is.
Some hospitals are starting pharmacist-led programs to monitor theophylline patients. One program cut hospitalizations by 37%. It’s not fancy. It’s just asking: “What else are you taking?”
The bottom line: Theophylline is still a powerful tool. But it’s not a set-it-and-forget-it drug. It needs attention. If you’re on it, treat it like insulin - a medication that demands careful, ongoing management. Because when metabolism slows down, the difference between healing and harm is just one pill away.
Can I take ibuprofen with theophylline?
Yes, ibuprofen doesn’t significantly affect theophylline clearance. It’s generally safe to use together. But always check with your doctor if you’re on multiple medications - some pain relievers like naproxen or celecoxib have less clear data, and high doses over long periods may still pose risks.
How long does it take for theophylline levels to change after stopping an interacting drug?
After stopping a CYP1A2 inhibitor like cimetidine or fluvoxamine, theophylline clearance typically returns to normal within 3 to 7 days. But levels don’t drop immediately - they decline gradually. That means your dose may need to be increased during this period to avoid losing control of your breathing. Always check your serum level before adjusting.
Is theophylline still used today?
Yes, but less often. It’s mostly used for severe asthma or COPD when newer inhalers don’t work, or in areas where cost limits access to newer drugs. Global sales were $187 million in 2022, with higher use in Asia and Africa. In the U.S., it’s now used in under 2% of COPD patients, but it still has a critical role for specific cases.
Do all antibiotics affect theophylline?
No. Only certain macrolides - erythromycin and clarithromycin - reduce clearance. Azithromycin does not. Other antibiotics like amoxicillin, doxycycline, or ciprofloxacin have little to no effect. Always ask which antibiotic you’re getting - and whether it’s safe with theophylline.
Why is theophylline toxicity so dangerous?
Theophylline affects the heart and nervous system. Toxic levels can cause dangerous heart rhythms (like ventricular tachycardia), seizures, or even cardiac arrest. It’s not just uncomfortable - it’s life-threatening. That’s why even a small increase in serum level, like from 18 to 25, can require emergency treatment.
Most people never hear about theophylline until they’re on it. And by then, it’s too late to learn the rules. The key is prevention. Know your meds. Talk to your pharmacist. Get your blood tested. One conversation could keep you out of the hospital.


Patrick Jarillon
7 February / 2026Let me tell you something they don't want you to know - theophylline isn't being phased out because it's dangerous. It's being phased out because Big Pharma doesn't make enough money off it. You think fluvoxamine is the problem? Nah. The real villain is the patent expiration. They replaced a $0.10 pill with a $30 inhaler and called it 'innovation.' I've seen patients on theophylline for 30 years - stable, alive, breathing - and then some 'expert' tells them to switch. Within weeks? ER visits. Coincidence? I think not.
And don't even get me started on 'pharmacist-led programs.' That's just a fancy way of saying 'we're outsourcing your care to someone who gets paid minimum wage to ask if you take Tums.' They don't even know what CYP1A2 stands for. But hey, at least the EHR says 'warning' in yellow. Like that's gonna stop a 72-year-old from taking Tagamet because her stomach burns.
Smoking increases clearance? Sure. But did you know nicotine patches do too? No one talks about that. Because it doesn't fit the narrative. The truth? The system is rigged. And theophylline? It's the last medicine that still listens to the patient - not the algorithm.