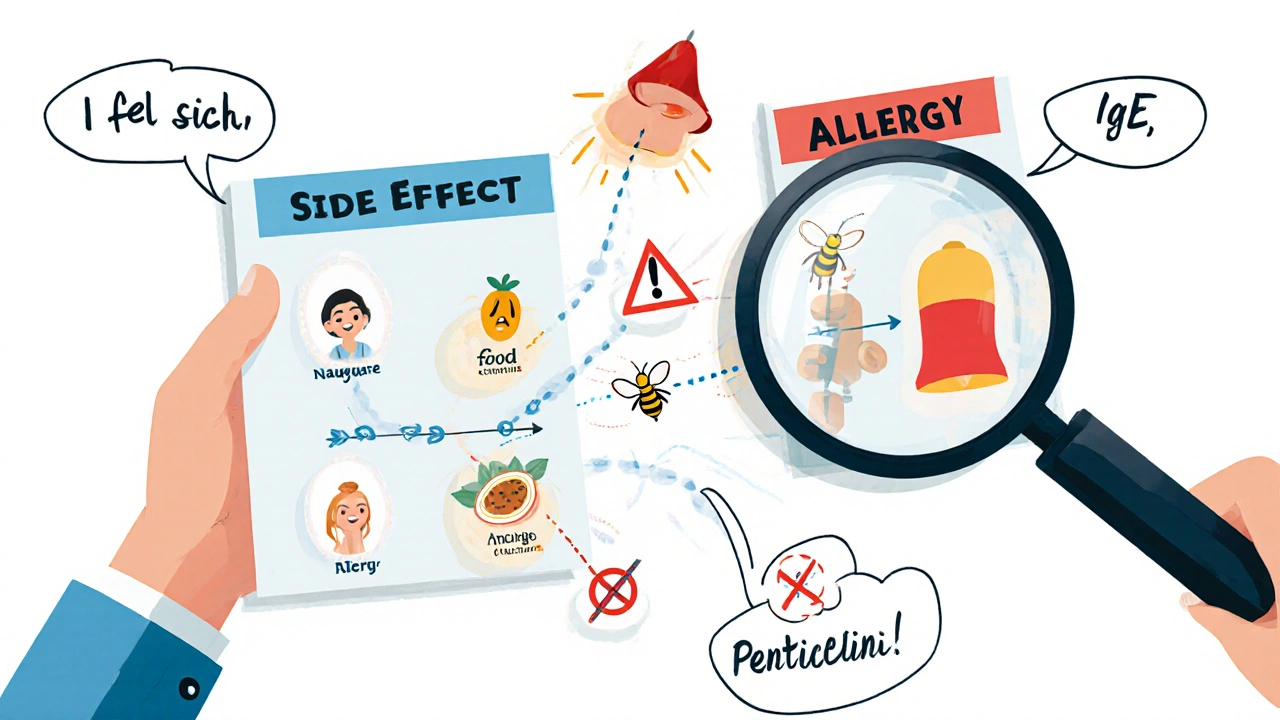
It’s easy to think that if a drug makes you feel sick, you’re allergic to it. But that’s not always true. In fact, most people who say they’re allergic to a medication aren’t. They’re just experiencing a side effect - something completely different from a real drug allergy. Confusing the two can lead to worse health outcomes, higher costs, and even life-threatening mistakes. Understanding the difference isn’t just useful - it’s essential.
What Are Medication Side Effects?
Side effects are predictable, non-allergic reactions that happen because of how a drug works in your body. Every medication has a purpose - to lower blood pressure, kill bacteria, reduce inflammation - but it doesn’t just target one part of your system. It affects others too. That’s where side effects come from.
For example, statins help lower cholesterol, but about 5-10% of people taking them get muscle aches. Metformin, used for diabetes, causes stomach upset in 20-30% of users. These aren’t random. They’re documented. The FDA requires drug labels to list these reactions with exact percentages. If a drug says, “Nausea occurs in 15% of patients,” that’s not a guess - it’s based on clinical trials.
Side effects usually show up within hours or days of starting the drug. They often get better over time. Your body adjusts. About 70-80% of common side effects fade within two to four weeks. You can often manage them too. Taking metformin with food cuts stomach issues in 60% of people. Lowering the dose helps with many side effects. Sometimes, switching to a similar drug works - like changing from lisinopril to another blood pressure pill if you get a dry cough.
What Is a True Drug Allergy?
A drug allergy is your immune system overreacting. It sees the medication as an invader - like a virus or pollen - and launches a defense. That’s not a side effect. That’s an allergic reaction. And it’s dangerous.
The immune system uses specific tools for this. In immediate reactions, IgE antibodies trigger symptoms within minutes to two hours. Think hives, swelling, trouble breathing, or anaphylaxis - a full-body crisis that can kill. Delayed reactions, caused by T-cells, show up days later. They often look like rashes - red, itchy patches that spread across the skin.
Penicillin is the most common trigger. About 80% of all serious drug allergies involve it. But sulfonamides, NSAIDs, and some seizure meds can cause them too. Unlike side effects, allergic reactions happen at normal doses. You don’t need to take more to get one. And they don’t go away with time. Once your immune system decides a drug is dangerous, it remembers. Even one tiny dose can set off a reaction again.
How to Tell the Difference
Here’s the key: side effects are about pharmacology. Allergies are about immunology.
Side effects are dose-dependent. Take more of a painkiller? Higher risk of stomach bleeding. Take less? Less nausea. Allergic reactions? They happen at any dose - even a tiny amount. That’s why people who think they’re allergic to penicillin after a rash from childhood might still react badly to a single pill decades later.
Timing matters too. If you got a headache and dizziness the day after starting a new pill? Probably a side effect. If you broke out in hives and your throat swelled up 15 minutes after swallowing it? That’s an allergy. A rash that showed up a week later? Likely a delayed allergic reaction.
And here’s the biggest clue: side effects can be managed. Allergies require avoidance. You can’t just “get used to” a true allergy. You have to avoid the drug - and sometimes others like it. For example, if you’re allergic to penicillin, you may also need to avoid amoxicillin and other penicillin-type antibiotics.
Why It Matters: The Real Cost of Mistakes
Here’s the scary part: up to 90% of people who say they’re allergic to penicillin aren’t. That’s not a typo. Studies from Brigham and Women’s Hospital and JAMA Internal Medicine show that when these patients get tested, most turn out to be fine. But they still avoid penicillin - and doctors give them stronger, broader antibiotics instead.
That’s a problem. Broader antibiotics kill more good bacteria. They increase the risk of dangerous infections like MRSA. One study found that mislabeling a penicillin allergy raises the chance of MRSA by 69%. It also adds $4,000 in extra costs per patient each year because of longer hospital stays and pricier drugs.
It’s not just penicillin. People say they’re allergic to ibuprofen because they got a stomachache. They blame statins for fatigue. They call diarrhea from amoxicillin an “allergy.” But those are side effects - not immune responses. And avoiding the right drug because of a mislabel can mean worse outcomes. One 2022 study in the Annals of Internal Medicine found that 40% of patients with mislabeled allergies had treatments delayed or limited because doctors thought they couldn’t use safe, effective options.
How Doctors Test for True Allergies
If you think you have a drug allergy, don’t just assume. Get tested. Skin tests are the gold standard for penicillin allergies. They’re 97% accurate at ruling out true allergies. If the skin test is negative, doctors often do an oral challenge - giving a small, controlled dose under supervision. The reaction rate in low-risk patients is just 0.2%.
For other drugs, newer tests like the basophil activation test (BAT) are now FDA-approved. It measures immune cell activity in the blood and is 85-95% accurate. Blood tests for IgE antibodies also help, especially when skin testing isn’t possible.
But testing isn’t common. Only 10% of U.S. allergists can handle drug allergy evaluations. That’s why many primary care doctors are now being trained to use simple tools like the PEN-FAST rule - a quick questionnaire that helps decide who’s safe to test. Patients who score low on PEN-FAST have a 99.8% chance of being able to safely take penicillin.

What You Should Do
If you’ve ever said, “I’m allergic to this drug,” ask yourself: Did you have a rash, swelling, or trouble breathing? Or did you just feel nauseous, tired, or have diarrhea? Write it down. Be specific. Include timing. Did it happen right after taking the pill? Or after a week? Did you need emergency care?
Bring that info to your doctor. Ask: “Could this have been a side effect?” If you’ve been told you’re allergic to penicillin or another common drug, ask about testing. Many hospitals now offer allergy clinics that specialize in this. Even if you’ve avoided a drug for years, you might be able to take it safely again.
And if you’re a parent, caregiver, or someone managing multiple medications - especially if you’re over 65 - this is critical. Older adults are three times more likely to have adverse drug reactions. Mislabeling allergies can lead to dangerous gaps in treatment. Don’t let a misunderstanding put you at risk.
What’s Changing in Medicine
Doctors are waking up to this problem. In 2018, only 15% of U.S. hospitals had programs to review and correct drug allergy labels. By 2023, that jumped to 65%. Academic hospitals are leading the way - 85% now have formal allergy clarification programs.
Electronic health records are helping too. Alerts now pop up when a patient has a vague allergy note like “allergic to antibiotics.” They prompt doctors to dig deeper. One study showed that after adding these alerts, documentation accuracy improved by 40-60%.
And the future? Personalized medicine. We now screen for the HLA-B*57:01 gene before giving abacavir (an HIV drug). That one test cuts allergic reactions from 8% to 0.4%. Similar tests are coming for other drugs. Soon, your DNA might tell your doctor which medications are safe - and which could trigger an immune response.
The bottom line: side effects are inconvenient. Allergies are dangerous. But the biggest danger isn’t the drug - it’s the mistake we make about what it’s doing to us.
Can you outgrow a drug allergy?
Yes, you can outgrow a drug allergy - especially penicillin. Studies show that about 80% of people who had a true penicillin allergy in childhood lose it over time, even without testing. But you shouldn’t assume it’s gone. Always get tested before trying the drug again. A simple skin test or oral challenge can confirm whether your immune system still reacts.
Is a rash always a sign of a drug allergy?
Not always. Rashes can be side effects too. Some drugs cause harmless, non-allergic skin rashes - especially antibiotics like amoxicillin. In fact, up to 10% of people taking amoxicillin develop a rash, but only a small fraction are allergic. The key is timing and symptoms. If the rash is itchy, spreads quickly, and comes with swelling or breathing trouble, it’s likely allergic. If it’s flat, not itchy, and appears after several days without other symptoms, it’s probably not.
Can you have a side effect without knowing the drug caused it?
Absolutely. Many side effects are vague - fatigue, dizziness, mild nausea - and people assume they’re due to stress, aging, or another illness. That’s why it’s important to track when symptoms start after beginning a new medication. If you felt fine before and felt off after starting a drug, that’s a red flag. Talk to your doctor. Don’t wait for a crisis to connect the dots.
Are over-the-counter drugs safe if you have drug allergies?
Not necessarily. Many OTC drugs contain the same active ingredients as prescription ones. If you’re allergic to penicillin, avoid amoxicillin - which is also in some OTC antibiotics. If you’re allergic to NSAIDs like ibuprofen, avoid aspirin or naproxen too. Always check labels. And if you’re unsure, ask your pharmacist. They can spot hidden cross-reactive ingredients.
What should I do if I think I’m having an allergic reaction?
Stop taking the drug immediately. If you have trouble breathing, swelling of the face or throat, dizziness, or a rapid heartbeat, call 911 or go to the ER. These are signs of anaphylaxis - a medical emergency. Don’t wait to see if it gets better. If you have an epinephrine auto-injector, use it right away. Afterward, see an allergist to confirm whether it was a true allergy and get proper documentation.
Can you be allergic to a drug you’ve taken before without problems?
Yes. Allergies can develop after repeated exposure. Your immune system doesn’t always react the first time. It needs to be sensitized - like how someone might develop a pollen allergy after years of exposure. So even if you’ve taken penicillin five times without issue, you could still have an allergic reaction on the sixth. That’s why you never assume safety based on past use.
Does having one drug allergy mean I’ll have more?
Not necessarily. Having one drug allergy doesn’t mean you’re prone to others. But people with multiple allergies - especially to different drug classes - may have a more reactive immune system overall. It’s rare, but if you’ve had two or more true allergic reactions, talk to an allergist. They can help identify patterns and guide safer choices.
Can I take a drug if I’m allergic to a similar one?
Sometimes - but only after testing. For example, if you’re allergic to penicillin, you might still tolerate a cephalosporin, especially newer ones. But the risk isn’t zero. Cross-reactivity depends on chemical structure. Only a specialist can determine if it’s safe. Never assume. Always get evaluated before trying a related drug.



Tina Dinh
29 November / 2025OMG I just realized I’ve been calling my amoxicillin rash an ‘allergy’ for years 😅 I got it after 3 days, no swelling, just a weird red patch-turns out it’s super common?! Time to book that skin test 🙌