Storing medications properly isn’t just a best practice-it’s a matter of life and death. If your insulin freezes, your asthma inhaler gets too hot, or your antibiotics sit in a humid bathroom cabinet, they might not work when you need them most. And it’s not just about personal use. Pharmacies, hospitals, and clinics face the same risks, with temperature and humidity control being the single biggest factor in whether a drug saves a life or becomes dangerous waste.
Why Temperature and Humidity Matter
Medications aren’t like canned food. They’re complex chemical formulas, often built around proteins or delicate compounds that break down when exposed to heat, moisture, or freezing. The active ingredient in your blood pressure pill, your diabetes medication, or your cancer treatment can lose potency if stored outside its narrow comfort zone. According to the FDA, nearly 78% of drug recalls in 2022 were linked to temperature excursions during storage or transport. That’s not a small number-it’s a systemic failure. Humidity is just as damaging. Too much moisture causes tablets to swell, capsules to soften, and powders to clump. It can also trigger chemical reactions that turn a safe drug into a toxic one. The World Health Organization says about 15-20% of global medication waste comes from poor storage conditions. That’s $35 billion worth of pills, syringes, and vials thrown away every year because someone didn’t know how to keep them dry.What Are the Right Conditions?
There’s no one-size-fits-all answer, but most medications fall into four standard categories defined by the U.S. Pharmacopeia (USP Chapter 1079):- Room Temperature: 20°C-25°C (68°F-77°F). This is the sweet spot for most pills, creams, and oral liquids. Brief excursions between 15°C-30°C (59°F-86°F) are usually okay, but not for long.
- Controlled Cold: 2°C-8°C (36°F-46°F). This is for insulin, many vaccines, biologics, and some antibiotics. Refrigerators in homes and clinics must hit this range exactly.
- Frozen: -25°C to -10°C (-13°F to 14°F). Used for certain long-term storage of vaccines and specialty drugs.
- Deep Frozen: Below -20°C (-4°F). Reserved for very sensitive products like some gene therapies.
Humidity? Aim for 50% relative humidity. The WHO says this is the ideal level to prevent degradation without drying out the product. Too dry? Tablets crack. Too wet? Mold grows. Both ruin the medicine.
Where Not to Store Medications
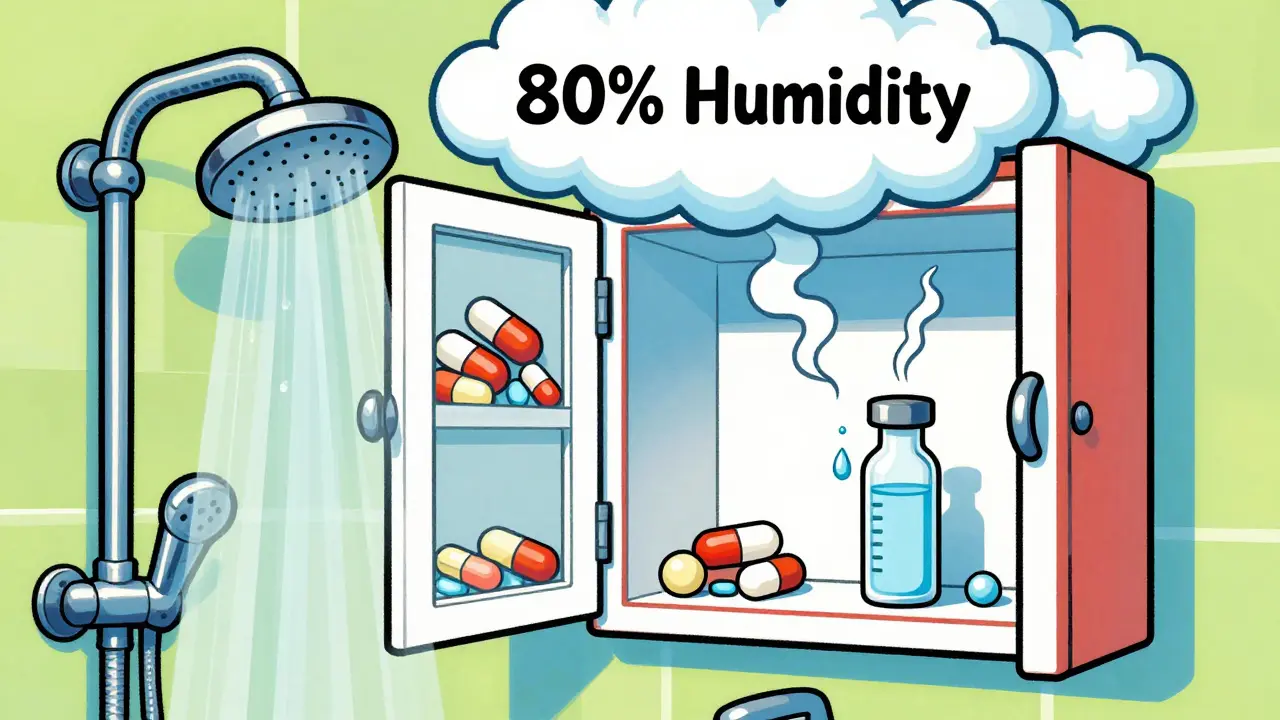
Common sense doesn’t always win in homes. Here’s where you should NEVER keep your meds:- Bathrooms: Steam from showers and sinks can spike humidity to 80% or higher. Even if the cabinet looks dry, moisture is hiding in the air.
- Kitchens: Near the stove, oven, or even the fridge? Heat rises. A pill on a counter above the microwave might hit 40°C (104°F) on a summer day.
- Windowsills: Sunlight heats surfaces fast. UV rays can also break down light-sensitive drugs like nitroglycerin or birth control pills.
- Car glove compartments: In Darwin, where summer temps hit 35°C+ daily, a car interior can hit 60°C (140°F). That’s not storage-that’s destruction.
- Freezers: Unless the label says “freeze,” don’t do it. Insulin, for example, becomes useless if frozen-even once.
Storing meds in a cool, dark closet or bedroom drawer is usually safest. If you’re unsure, check the packaging. Most manufacturers print storage instructions right on the box or leaflet.
How Storage Units Fail
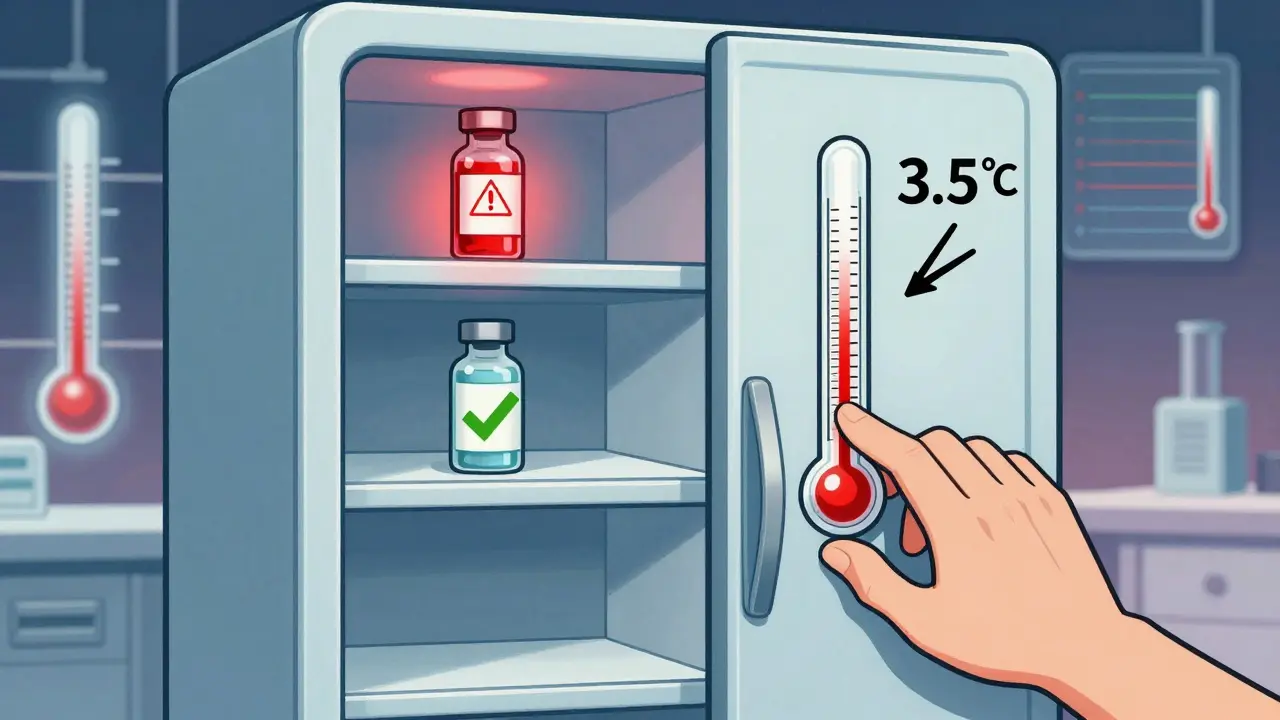
Even if you have a fridge or cabinet labeled “medication storage,” it might not be working right. A 2022 study by Helmer Scientific found that standard pharmacy refrigerators can have a 3.5°C (6.3°F) difference between the top shelf and the bottom. That means your insulin on the top shelf could be at 10°C while the one below is at 6.5°C-both are technically “in range,” but one is heading toward failure. Door storage is another trap. The temperature swings near fridge doors average 2.8°C (5°F) higher than the center. That’s why the CDC recommends storing vaccines in the middle of the unit, not on the door. Same goes for home fridges. Put your insulin in the back, on the middle shelf, away from the cooling vent. And don’t assume your fridge is cold enough. Many home fridges run at 6°C-8°C, which is okay for insulin-but if the thermostat is off by just 1°C, you’re already in danger. That’s why monitoring matters.Monitoring: The Missing Piece
You can’t manage what you don’t measure. A 2023 analysis of 15,000 pharmacy temperature logs showed that 18.7% of pharmacies had at least one temperature excursion above 77°F during summer months. The average time the meds were exposed? Over four hours. Simple thermometers won’t cut it. You need a data logging device (DDL) with:- A buffered probe (not a bare sensor)
- Alarm alerts for out-of-range temps
- Minimum and maximum temperature tracking
- Calibration certificate (valid for at least one year)
- Logging every 30 minutes or less
Most pharmacies still use outdated tools. Polygon Group’s 2023 study found that 73% of facilities had inadequate monitors, and 41% used non-buffered probes. These give false readings when the door opens-making staff think everything’s fine when it’s not.
Now, the FDA is stepping in. By December 2025, all healthcare facilities storing temperature-sensitive drugs must have real-time remote monitoring. That means alerts sent to your phone or computer if the fridge goes out of range. No more guessing. No more delays.

What Happens When Things Go Wrong
Exposure to heat or humidity doesn’t always make medicine look different. You can’t see the degradation. But you can feel the effects. A 2022 study by Dr. Michael Chen at Baystate Health showed that drugs stored outside the 59°F-77°F range lost 23%-37% of their potency. Hormone-based drugs like birth control pills, thyroid meds, and chemotherapy agents were the worst affected. A patient taking a weakened birth control pill might not realize it until she gets pregnant. A cancer patient on a degraded chemo drug might not get the dose needed to kill the tumor. And it’s not just personal risk. When a pharmacy dispenses a batch of degraded antibiotics, it can lead to treatment failure, longer hospital stays, and even antibiotic resistance.How to Fix It
If you’re a patient: Use a small, dedicated cooler with a temperature monitor for travel. Keep meds in your carry-on, not checked luggage. Never leave them in a car. If you suspect your meds were exposed to extreme temps, don’t use them-call your pharmacist. If you run a clinic or pharmacy: Invest in a proper DDL. Train staff to check logs daily. Never store meds in bathrooms, kitchens, or near windows. Keep a backup power source for refrigerators. Document every temperature reading. The Joint Commission says 62% of storage deficiencies in 2022 came from failing to follow manufacturer instructions. Don’t be part of that statistic. If you’re in a low-resource setting: The WHO reports only 28% of healthcare facilities in developing countries have adequate monitoring. Simple solutions exist-like insulated boxes with phase-change materials that maintain 2°C-8°C for up to 120 hours without electricity. These are being piloted now. Ask your local health authority if they’re available.The Future of Medication Storage
Technology is catching up. Blockchain-based tracking, used by Pfizer and Moderna in 2023, records every temperature change from factory to patient with 99.98% accuracy. AI systems, like those from Polygon Group, predict excursions before they happen-cutting failures by 76% in tests. Passive cooling packs are now standard in vaccine shipments. By 2027, 85% of storage facilities will use IoT sensors that auto-report to the cloud. But none of this matters if we ignore the basics. No sensor replaces common sense. No app fixes a fridge that’s too full or placed next to a radiator. The most powerful tool you have is knowing the rules-and following them.Can I store all medications in the fridge?
No. Only medications labeled for refrigeration should go in the fridge. Many pills, creams, and liquids can be damaged by cold temperatures. Always check the label. Insulin, vaccines, and certain antibiotics are common fridge items-but even insulin can be ruined if it freezes. Never assume a fridge is safe without checking the temperature range.
How often should I check the temperature of my medication storage?
At least once a day. If you’re using a data logger, review the log daily. If you’re using a manual thermometer, check it morning and night. In high-risk settings like clinics or pharmacies, logs should be reviewed and signed off by staff each shift. Temperature excursions can happen overnight, during power outages, or after a door is left open.
What should I do if my medication was left in a hot car?
Do not use it. Even if it looks normal, heat can permanently damage the active ingredients. Contact your pharmacist or prescribing provider. They can advise if you need a replacement. For critical medications like insulin or epinephrine, don’t wait-get a new supply immediately. The risk of taking a degraded drug is far greater than the cost of a replacement.
Is humidity really that big of a deal for pills?
Yes. High humidity causes tablets to absorb water, which can change how they dissolve in your body. It can also cause capsules to stick together or leak. In extreme cases, moisture triggers chemical reactions that turn safe drugs into harmful ones. The ideal humidity level is 50%. Bathroom cabinets often hit 70-80%-that’s why they’re unsafe.
Do I need a special fridge for medications?
Not necessarily, but a standard home fridge often isn’t reliable enough. Home fridges fluctuate too much, especially near the door or freezer compartment. A dedicated medical fridge with a temperature monitor is best for clinics. For home use, get a small, portable fridge with a built-in thermometer and keep it in a stable location-away from the kitchen heat and direct sunlight. Always verify the temperature with a calibrated monitor, not just the fridge’s display.


Maranda Najar
22 February / 2026Let me tell you something that keeps me up at night: the sheer, unadulterated negligence in how we treat life-saving medicine. It’s not just about refrigerators-it’s about societal collapse wrapped in pharmaceutical packaging. I’ve seen insulin vials left on dashboards in 110-degree heat, and I’ve watched elderly patients swallow crumbling tablets because they couldn’t afford to replace them. This isn’t science. This is tragedy dressed in clinical jargon. The FDA’s 78% recall statistic? That’s not a number-it’s a funeral dirge for every person who trusted the system and got betrayed. We’ve normalized neglect as convenience. And someone has to say it: this is moral failure, not logistical error.