Some medications are like walking a tightrope. One tiny misstep in dosage - even 5% off - can mean the difference between healing and hospitalization. These are NTI drugs: Narrow Therapeutic Index medications. They don’t play nice with guesswork. A little too much, and you risk toxicity. A little too little, and the treatment fails. There’s no room for error. If you’re taking one of these, or caring for someone who is, understanding which drugs fall into this category isn’t just helpful - it’s life-saving.
What Exactly Makes a Drug an NTI Drug?
An NTI drug has a very small window between the dose that works and the dose that harms. Think of it like a thermostat set to 72°F. If it jumps to 75°F, your house gets too hot. Drop to 69°F, and you’re shivering. For NTI drugs, that temperature range is measured in nanograms per milliliter of blood. For example, digoxin - used for heart rhythm problems - has a therapeutic range of just 0.5 to 2.0 ng/mL. Go above 2.0, and you could develop dangerous heart arrhythmias. Fall below 0.5, and your heart condition won’t be controlled.
The FDA defines NTI drugs as those where small changes in blood concentration can lead to serious, even life-threatening, outcomes. It’s not just about potency. It’s about precision. That’s why generic versions of these drugs aren’t treated the same as others. While most generics only need to match the brand-name drug within 80-125% of its absorption, NTI generics must stay within 90-111%. That tighter standard exists for a reason: switching brands or generics without monitoring can throw patients into danger.
Top NTI Drugs You Need to Know
Here’s a clear, practical list of the most common NTI drugs in use today, grouped by therapeutic class. These aren’t theoretical - they’re prescribed daily across hospitals, clinics, and homes.
- Anticoagulants: Warfarin (Coumadin) is the classic example. Its target INR is 2.0-3.0 for most conditions. A single INR of 4.0 or higher increases major bleeding risk by over 7 times. Even a small change in diet, antibiotics, or supplements can swing INR levels dangerously.
- Cardiac Drugs: Digoxin (Lanoxin), flecainide, and procainamide all require strict blood level monitoring. Digoxin’s margin is so narrow that a missed dose or a kidney issue can trigger toxicity within hours.
- Antiepileptics: Phenytoin (Dilantin), carbamazepine (Tegretol), and valproic acid (Depakote) are critical for seizure control. Phenytoin’s therapeutic range is 10-20 mcg/mL. Levels above 20 can cause slurred speech, tremors, and even coma.
- Immunosuppressants: Tacrolimus, cyclosporine, and sirolimus are used after organ transplants. If levels drop, the body rejects the new organ. If they rise too high, kidneys fail or nerves are damaged. Trough levels for tacrolimus are typically kept between 5-15 ng/mL - and checked 3 times a week in the first month post-transplant.
- Psychiatric Medications: Lithium is the most well-known. Therapeutic range: 0.6-1.2 mmol/L. At 1.5 mmol/L, you’re in toxic territory - vomiting, confusion, and seizures can follow. Many patients miss monitoring appointments, and that’s when problems arise. Nortriptyline, a tricyclic antidepressant, also falls here with a range of 50-150 ng/mL.
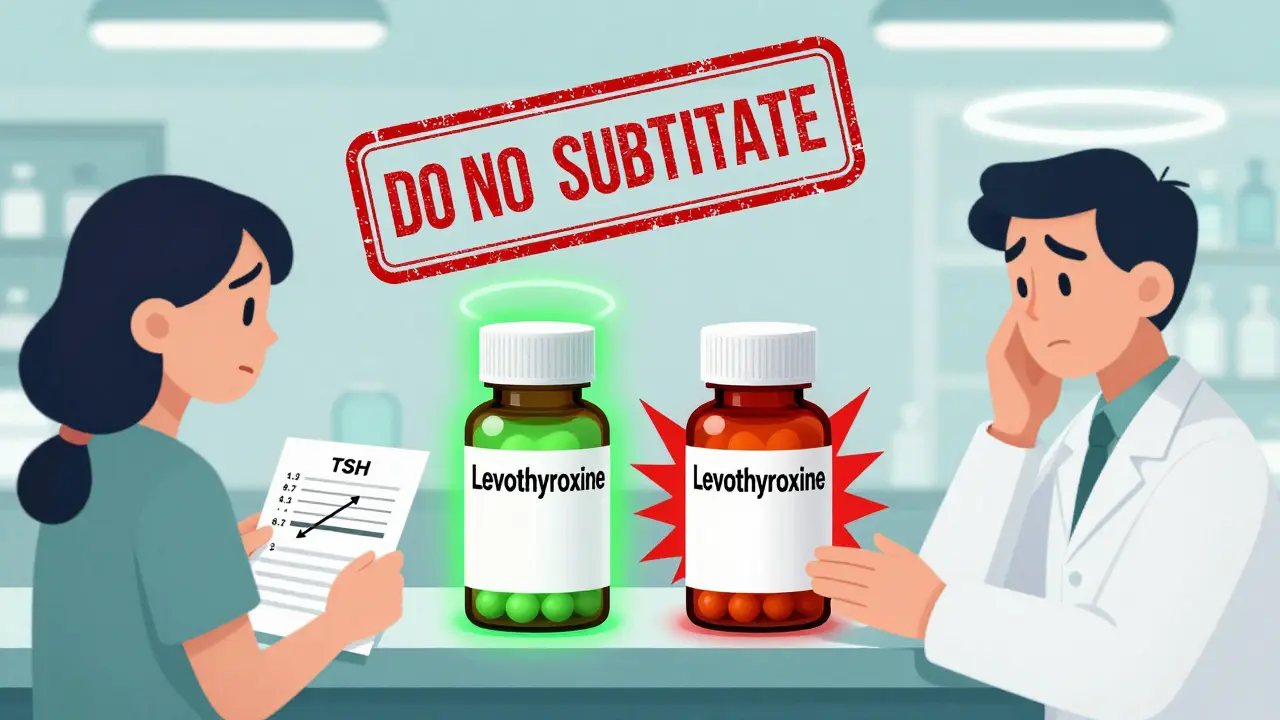
- Thyroid Hormone: Levothyroxine (Synthroid, Tirosint) is often overlooked as an NTI drug. But small changes in dose can cause TSH levels to swing from 1.2 to 8.7 mIU/L - as seen in real cases where patients switched generics. That’s not just a lab number; it’s fatigue, weight gain, or heart palpitations.
- Antibiotics: Aminoglycosides like gentamicin and tobramycin require peak and trough monitoring. Peak levels must hit 5-10 mcg/mL to kill bacteria, but troughs must stay below 2 mcg/mL to avoid kidney and ear damage.
- Emerging Cancer Drugs: New targeted therapies like axitinib, ponatinib, and olaparib are now classified as NTI. Their therapeutic ranges are narrow because they’re designed to attack specific cancer cells - but they also hit healthy ones if levels creep up.
Why Generic Switching Can Be Risky
Many people assume all generics are interchangeable. That’s true for most drugs - but not for NTI drugs. A 2023 Reddit thread from a pharmacist described a 62-year-old woman whose TSH jumped from 1.2 to 8.7 after her pharmacy switched her levothyroxine brand. She didn’t feel different at first. Then she developed heart palpitations and weight gain. It took three months of dose adjustments to get back to normal.
That’s not rare. Studies show that even slight differences in fillers, coatings, or absorption rates between generic brands can cause clinically significant changes in blood levels of NTI drugs. That’s why 47 U.S. states have laws restricting automatic substitution. In 28 of them, a doctor must specifically write “Dispense as Written” or “Do Not Substitute” on the prescription. Without that note, the pharmacist might legally switch the brand - putting the patient at risk.
Monitoring Isn’t Optional - It’s Mandatory
If you’re on an NTI drug, regular blood tests aren’t a suggestion. They’re part of the treatment plan. Here’s what monitoring looks like for the most common ones:
- Warfarin: INR checked every 3-5 days after starting, then weekly until stable, then monthly.
- Lithium: Blood levels checked every 3-6 months, or after any dose change or illness.
- Phenytoin: Trough levels checked at least once every 2-3 months, more often if kidney or liver function changes.
- Tacrolimus: Trough levels checked 3x per week in the first month after transplant, then weekly, then monthly.
- Levothyroxine: TSH tested every 6-8 weeks after a dose change, then annually if stable.
But here’s the problem: only 45% of hospital systems have automated alerts when NTI drug levels go out of range. Many patients forget appointments. Some can’t afford the tests - which cost $25 to $150 per draw. Medicare covers 80%, but the rest falls on the patient. That’s why adherence rates for lithium monitoring are as low as 68%, according to JAMA Internal Medicine.
What You Can Do to Stay Safe
If you’re on an NTI drug, here’s your action plan:
- Know your drug’s name and purpose. Don’t just take it - understand why it’s different.
- Ask your doctor if your drug is NTI. Many patients don’t realize they’re on one.
- Request “Dispense as Written” on your prescription if switching brands worries you.
- Keep a log of your lab results. Track your INR, TSH, lithium level - don’t rely on memory.
- Report any new symptoms. Dizziness, nausea, irregular heartbeat, tremors, or confusion could signal toxicity.
- Don’t start new supplements or OTC meds without checking. St. John’s wort, aspirin, and even some antacids can interfere.

The Future of NTI Drug Management
The field is changing. The FDA is expanding its list of NTI drugs to include newer anticoagulants like apixaban and rivaroxaban - even though some experts argue their windows are wider. Meanwhile, AI-driven monitoring systems are being tested in hospitals. One pilot study across 12 centers cut NTI-related adverse events by 28% by predicting dangerous dose changes before they happened.
Long-term, pharmacogenomics - testing how your genes affect drug metabolism - is showing promise. The NIH is funding a $15 million study on using genetic markers to personalize warfarin and phenytoin dosing. Early results show patients reach safe, effective levels 40% faster than with standard dosing.
But technology alone won’t fix the problem. The real challenge is access. People in low-income areas, rural communities, or without consistent insurance still struggle to get regular monitoring. Until that changes, the risk remains high - especially as more cancer drugs enter the NTI category.
Bottom Line
NTI drugs are powerful tools - but they demand respect. They’re not like antibiotics you take for a week and forget. They require ongoing attention, communication with your care team, and vigilance. If you’re on one, you’re not just a patient. You’re part of a precision system. Your next lab test could be the difference between staying well and facing a medical emergency. Stay informed. Stay involved. And never assume a generic is the same as your brand - unless your doctor says so.
Are all generic drugs unsafe for NTI medications?
No, not all generics are unsafe. But for NTI drugs, even small differences in absorption can matter. The FDA requires stricter bioequivalence standards (90-111%) for NTI generics compared to regular ones (80-125%). If your doctor approves a generic, it’s usually safe - but you should still monitor levels closely. Never switch brands without telling your provider.
Can I stop taking my NTI drug if I feel fine?
Never stop or change the dose of an NTI drug without medical supervision. Feeling fine doesn’t mean the drug isn’t working - or that your levels aren’t dangerously low or high. Many patients with epilepsy or heart conditions feel normal even when their drug levels are outside the therapeutic range. Stopping abruptly can trigger seizures, strokes, or organ rejection.
Why is lithium considered an NTI drug?
Lithium has a very narrow window between therapeutic and toxic levels. The safe range is 0.6-1.2 mmol/L. At 1.5 mmol/L, toxicity begins - with symptoms like tremors, vomiting, and confusion. Above 2.0 mmol/L, it can cause seizures, coma, or death. Kidney function, salt intake, and dehydration all affect lithium levels, making monitoring essential.
Is levothyroxine really an NTI drug?
Yes. Although it’s often treated as a simple hormone replacement, levothyroxine has a narrow therapeutic index. Small changes in dose can cause TSH levels to swing dramatically. A shift from 1.2 to 8.7 mIU/L - as seen in documented cases - can cause fatigue, weight gain, depression, or heart strain. Many states include it on their official NTI drug lists for this reason.
How often should I get blood tests for my NTI drug?
It depends on the drug and your condition. For warfarin, check INR every 3-5 days when starting, then weekly until stable. For lithium, every 3-6 months if stable. Tacrolimus requires testing 3 times a week after transplant. Always follow your provider’s schedule - and get tested sooner if you feel unwell, start new medications, or have illness or dehydration.


Glendon Cone
30 December / 2025This is one of those posts that makes you pause and think. I work in pharmacy and see this daily - people switching generics without realizing the risk. That levothyroxine case? I had a patient go from 1.1 to 9.8 TSH after a switch. No symptoms at first. Then she had atrial fibrillation. We had to admit her. Don't let 'it's just a generic' fool you. 🙏