NSAID Kidney Risk Calculator
This calculator estimates your risk of acute kidney injury from NSAID use based on key factors. It's designed for people concerned about kidney health.
Your Risk Assessment
Low Risk
Based on your inputs, your risk of acute kidney injury from NSAID use is low.
Key Recommendations:
Every year, tens of thousands of people end up in the hospital with sudden kidney damage - and many of them didn’t even know they were at risk. The culprit? Common painkillers like ibuprofen, naproxen, and aspirin. These drugs, sold over the counter in nearly every pharmacy and grocery store, are often seen as harmless. But for people with kidney disease or even just mild kidney stress, they can trigger acute kidney injury in as little as 48 hours.
How NSAIDs Actually Hurt Your Kidneys
NSAIDs work by blocking enzymes called COX-1 and COX-2, which help make prostaglandins. These prostaglandins aren’t just about inflammation - they’re critical for keeping blood flowing to your kidneys. When you take an NSAID, you cut off that signal. Your blood vessels tighten, your kidneys get less blood, and your filtering system slows down.
This isn’t theoretical. In people with healthy kidneys, a single dose might cause a small, temporary dip in kidney function - and that’s usually fine. But if you already have reduced kidney function, are dehydrated, are on blood pressure meds like ACE inhibitors or diuretics, or are older than 65, that dip can turn into a crash. Studies show NSAIDs can drop kidney filtration rates by 20% to 40% within a day in vulnerable people.
There’s also a less common but serious reaction called acute interstitial nephritis - your immune system mistakenly attacks kidney tissue. This can happen even after one or two doses, and it often shows up with fever, rash, or blood in the urine. Many patients don’t realize this is linked to their painkiller until it’s too late.
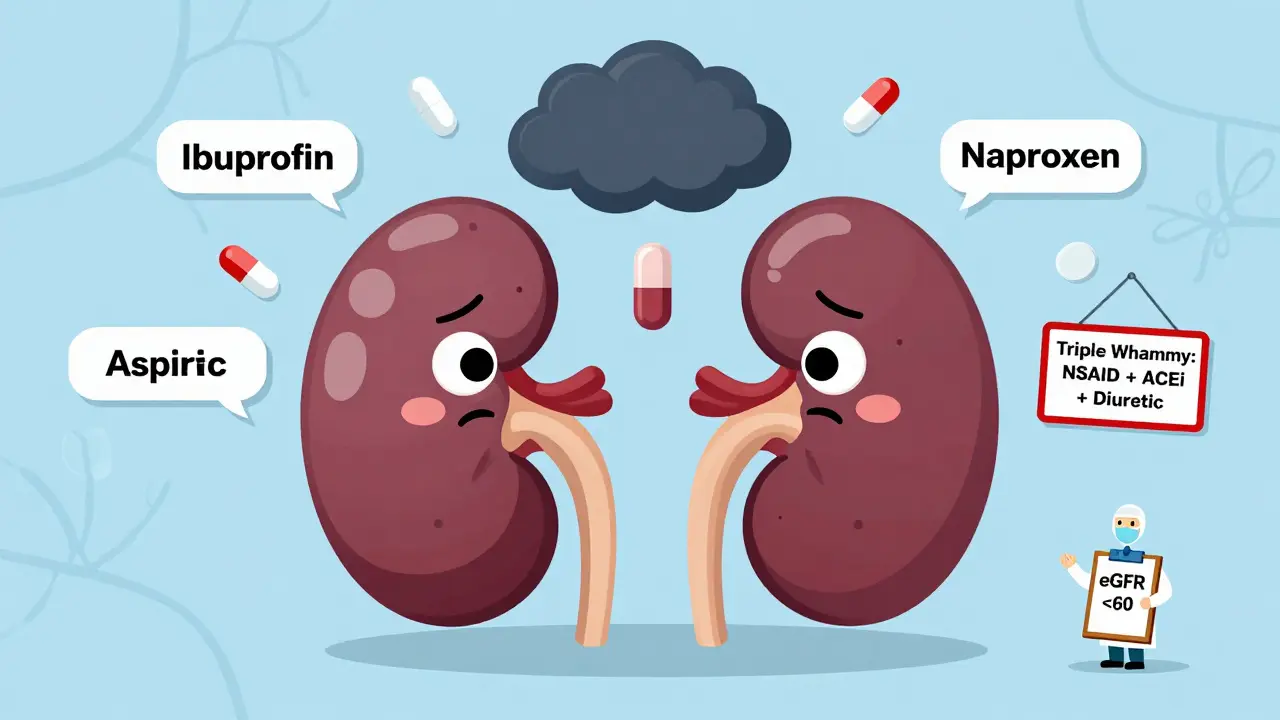
The Triple Whammy: A Deadly Combination
One of the most dangerous mistakes people make is stacking NSAIDs with other common meds. This is called the “triple whammy”: NSAID + ACE inhibitor or ARB + diuretic.
Here’s why it’s risky:
- Diuretics (like furosemide) pull fluid out of your body, lowering blood volume.
- ACE inhibitors and ARBs (like lisinopril or losartan) relax blood vessels, which lowers blood pressure.
- NSAIDs block the prostaglandins your kidneys need to compensate for both of those effects.
Together, they leave your kidneys with no backup plan. Research shows this combo increases the risk of acute kidney injury by 31% overall - and up to 82% in the first 30 days. That’s not a small risk. It’s a red flag.
Many patients don’t even know they’re on this combo. They take ibuprofen for arthritis, lisinopril for high blood pressure, and hydrochlorothiazide for swelling - all prescribed by different doctors. No one connects the dots.
Who’s Most at Risk?
Not everyone who takes NSAIDs gets kidney damage. But certain groups are far more vulnerable:
- People with eGFR below 60 - even mild kidney impairment doubles the risk.
- Those over 65 - kidney function naturally declines with age, and older adults are more likely to be on multiple medications.
- People with heart failure, liver disease, or diabetes - these conditions already strain kidney function.
- Anyone dehydrated - from illness, heat, or exercise. Marathon runners who take NSAIDs during races have a higher risk of sudden kidney shutdown.
- Chronic users - taking NSAIDs for weeks or months increases the chance of long-term kidney damage.
A 2023 study found that people with existing kidney disease who used NSAIDs regularly had a 50% higher chance of their condition worsening. For some, it meant moving from stage 3 to stage 4 chronic kidney disease in under a year.
What Are the Early Warning Signs?
Here’s the scary part: acute kidney injury often has no symptoms at first. By the time you feel tired, swollen, or notice less urine, damage may already be done.
But these signs should raise red flags:
- Less urine output than usual (especially under 400 mL per day)
- Swelling in ankles, feet, or hands
- Unexplained fatigue or nausea
- High blood pressure that’s suddenly harder to control
- Dark or foamy urine
One study found that 30% of patients with NSAID-induced kidney injury had no rise in serum creatinine - the standard blood test doctors use - until damage was already advanced. That’s why relying on one test can be misleading.
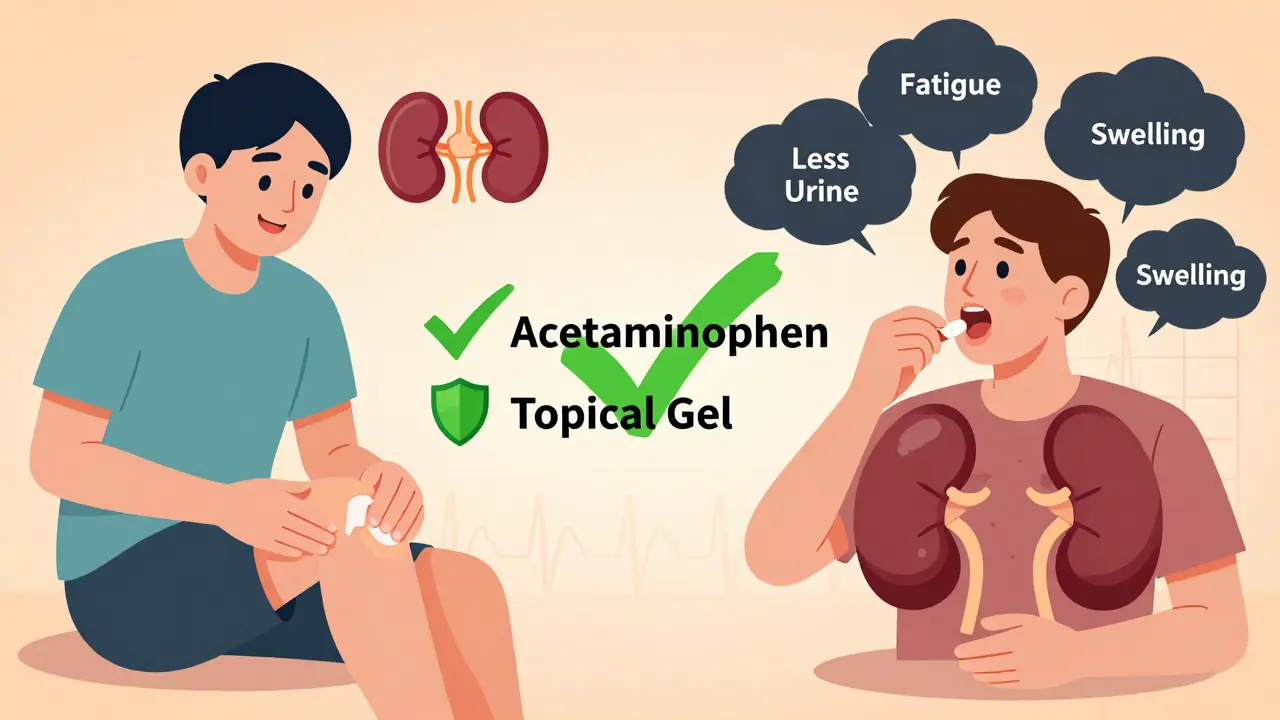
NSAIDs vs. Alternatives: What’s Safer?
If you need pain relief but have kidney concerns, here’s what works - and what doesn’t:
| Option | Kidney Risk | Anti-Inflammatory? | Best For |
|---|---|---|---|
| Acetaminophen (Tylenol) | Low - 40-50% lower risk than NSAIDs | No | Headaches, fever, mild joint pain |
| Topical NSAIDs (gel, patch) | Very low - 70-80% less systemic absorption | Yes | Localized pain (knee, shoulder, back) |
| Physical therapy / heat/cold | None | No | Chronic muscle or joint pain |
| Opioids | Minimal direct risk | No | Severe pain (short-term only) |
| Oral NSAIDs (ibuprofen, naproxen) | High - especially with risk factors | Yes | Avoid if eGFR <60 or on “triple whammy” meds |
Topical NSAIDs are a game-changer. A 2024 trial with 3,200 patients showed they were just as effective for joint pain as pills - but with half the kidney risk. If your pain is in one area, skip the pill and use a gel.
How to Protect Your Kidneys
If you’re at risk - or just want to be safe - follow these four steps:
- Know your eGFR. Ask your doctor for your kidney function number. If it’s below 60, NSAIDs should be avoided unless absolutely necessary.
- Avoid the triple whammy. Never take NSAIDs with ACE inhibitors, ARBs, and diuretics together. If you’re on any of these, talk to your doctor before using any painkiller.
- Use the lowest dose for the shortest time. For acute pain, stick to 3-5 days max. If pain lasts longer, see your doctor - don’t just keep taking pills.
- Stay hydrated. Drink 5-10 mL of water per kg of body weight before exercise or hot weather. During activity, aim for 0.4-0.8 liters per hour. This keeps your kidneys working and reduces NSAID risk by up to 60%.
Also, check your labels. Some cold and flu meds, menstrual relief pills, and sleep aids contain hidden NSAIDs. Read the “active ingredients” list - ibuprofen, naproxen, ketoprofen, diclofenac - they’re all the same family.
What’s New in Kidney Protection?
Science is catching up. In 2023, the American Society of Nephrology launched a free online NSAID-RF Risk Calculator. It takes 12 factors - age, blood pressure, meds, eGFR - and gives you a 30-day risk score. If it’s over 15%, NSAIDs are probably not worth the risk.
Researchers are also testing new drug combos. One trial is mixing ibuprofen with acetylcysteine - an antioxidant that may shield kidney cells. Early results show it keeps pain relief but cuts down on oxidative stress in the kidneys.
And soon, genetic testing might tell you if you’re extra sensitive to NSAIDs. A 2025 study found people with certain PTGS2 gene variants are 3x more likely to develop kidney injury from these drugs. Personalized medicine is coming - but it’s not here yet.
Real Stories, Real Consequences
On Reddit’s kidney health forums, hundreds of people share stories like this:
“I took 800mg ibuprofen for my back pain. Three days later, I couldn’t walk. My creatinine shot up to 4.1. I was hospitalized. No one warned me.”
That’s not rare. A 2022 survey of nephrologists found that 58% of their patients had no idea NSAIDs could hurt their kidneys. Many thought “over-the-counter” meant “safe for everyone.”
One 72-year-old man in Rhode Island took ibuprofen 800mg three times a day for arthritis. His eGFR was 58 - just below the danger line. Within 72 hours, it dropped to 22. He needed dialysis for a week. He’s still on medication. His kidney never fully recovered.
Final Thoughts: Safety Isn’t About Avoiding Pills - It’s About Awareness
NSAIDs aren’t evil. They help millions of people live with pain. But they’re not harmless either. The problem isn’t the drug - it’s the assumption that it’s safe for everyone.
If you have kidney disease, high blood pressure, diabetes, or are over 65 - don’t guess. Ask your doctor before taking any NSAID. Even if you feel fine, your kidneys might not be.
Know your numbers. Know your meds. Know your limits. A few simple questions could save your kidneys - and your future.
Can I take ibuprofen if I have mild kidney disease?
If your eGFR is between 30 and 60, NSAIDs like ibuprofen should be used with extreme caution - only at the lowest dose for the shortest time (no more than 3 days per week). Above all, avoid combining them with diuretics or ACE inhibitors/ARBs. For most people in this range, acetaminophen or topical NSAIDs are safer choices.
Does naproxen hurt the kidneys more than ibuprofen?
Both carry similar risks for kidney injury. Naproxen lasts longer in the body, so it may expose your kidneys to the drug for more hours each day. But ibuprofen is taken more frequently, which can lead to repeated stress. Neither is safer than the other - both should be avoided if you have reduced kidney function.
Is it safe to take NSAIDs after a workout?
It’s not recommended, especially if you’re dehydrated or exercising in heat. NSAIDs reduce blood flow to the kidneys, and intense exercise already stresses them. Studies show this combo can cut kidney blood flow by 30-50% beyond normal exercise levels. For recovery, use ice, stretching, or acetaminophen instead.
How do I know if NSAIDs damaged my kidneys?
The only reliable way is through blood and urine tests. Ask your doctor for an eGFR and urine albumin-to-creatinine ratio. Symptoms like swelling, fatigue, or less urine may appear late - sometimes after damage is already done. Don’t wait for symptoms to get tested.
Can kidney damage from NSAIDs be reversed?
If caught early - within days - kidney function often returns to normal after stopping the NSAID. But if injury lasts more than a week or leads to acute kidney failure, some damage may be permanent. The longer you wait, the higher the chance of chronic kidney disease developing.


Rich Robertson
15 December / 2025Man, I had no idea ibuprofen could wreck your kidneys like that. I’ve been popping 2 Advil after gym days for years thinking it was just helping me recover. Guess I’m switching to acetaminophen now - and drinking way more water. Thanks for the wake-up call.