Hypoglycemia Treatment Calculator
Use this tool to determine the correct amount of fast-acting carbs needed to treat hypoglycemia according to the 15-15 rule. This follows recommendations from diabetes treatment guidelines.
Enter your blood sugar and treatment choice to see recommended action.
Follow the 15-15 rule: take 15g fast-acting carbs, wait 15 minutes, then recheck blood sugar. Repeat if needed until above 70 mg/dL. Always follow up with a snack containing protein and complex carbs.
Low blood sugar isn’t just a nuisance-it can be dangerous. If you’re taking insulin, sulfonylureas, or meglitinides for diabetes, you’re at risk for hypoglycemia. Blood glucose below 70 mg/dL triggers symptoms like sweating, shaking, and confusion. Below 54 mg/dL, you could pass out or have a seizure. This isn’t rare. About 1 in 4 people with type 1 diabetes develop hypoglycemia unawareness after 15 years. And for those on insulin, it’s not unusual to experience 2-3 low blood sugar events every year.
Know Which Medications Put You at Risk
Not all diabetes drugs cause low blood sugar. Some are much safer than others. If you’re on insulin, you’re in the highest-risk group-20% to 40% of users have at least one hypoglycemic event each year. Sulfonylureas like glimepiride and glyburide are next, with 15% to 30% of users having lows annually. Meglitinides like repaglinide carry a 10% to 20% risk. These drugs force your pancreas to release insulin, even when you haven’t eaten.On the other hand, metformin, GLP-1 agonists (like semaglutide), and SGLT2 inhibitors (like empagliflozin) rarely cause hypoglycemia on their own. If you’re on one of these and still getting lows, check if you’re also taking insulin or a sulfonylurea. That’s usually the culprit.
Recognize the Warning Signs-Before It’s Too Late
Hypoglycemia has two phases: autonomic and neuroglycopenic. The first tells you something’s wrong. The second means your brain is starving.- Autonomic symptoms (below 70 mg/dL): Sweating, trembling, fast heartbeat, hunger, anxiety
- Neuroglycopenic symptoms (below 55 mg/dL): Confusion, dizziness, slurred speech, weakness, seizures, loss of consciousness
Here’s the problem: if you’ve had diabetes for a long time, your body stops sending those early warning signals. That’s called hypoglycemia unawareness. It affects 25% of type 1 patients after 20 years. If you don’t feel your lows coming, you’re at higher risk of passing out-especially at night.
Use the 15-15 Rule-But Do It Right
When your blood sugar drops below 70 mg/dL, treat it fast. The standard advice is the 15-15 rule: take 15 grams of fast-acting carbs, wait 15 minutes, then check again.But most people get it wrong. They reach for candy bars, juice boxes with sugar substitutes, or whole grain crackers. None of those work fast enough.
Use these instead:
- 4 glucose tablets (14g carbs total)
- 1/2 cup (4 oz) of regular soda (not diet)
- 1 tablespoon of honey or sugar
- Glucose gel (1 tube)
After 15 minutes, recheck your blood sugar. If it’s still below 70, repeat. Don’t eat a full meal yet-wait until your glucose is steady above 70. Then have a snack with protein and complex carbs (like peanut butter on toast) to prevent another drop.
Studies show 89% of mild to moderate lows are fixed correctly with this method-if you use the right carbs. But 63% of patients use the wrong ones, delaying recovery and increasing risk.
Prevent Nighttime Lows
Nocturnal hypoglycemia is scary-and common. About 2.3 times per week, on average, people on insulin wake up with sweating, nightmares, or confusion. Some don’t wake up at all.Here’s how to reduce the risk:
- Check your blood sugar before bed. If it’s below 100 mg/dL, eat a small snack with protein and fat (like cheese and crackers or a handful of nuts).
- Avoid alcohol at night. It blocks your liver from releasing glucose and can cause lows up to 12 hours later.
- If you exercised in the evening, reduce your evening insulin dose by 10%-20% (talk to your doctor first).
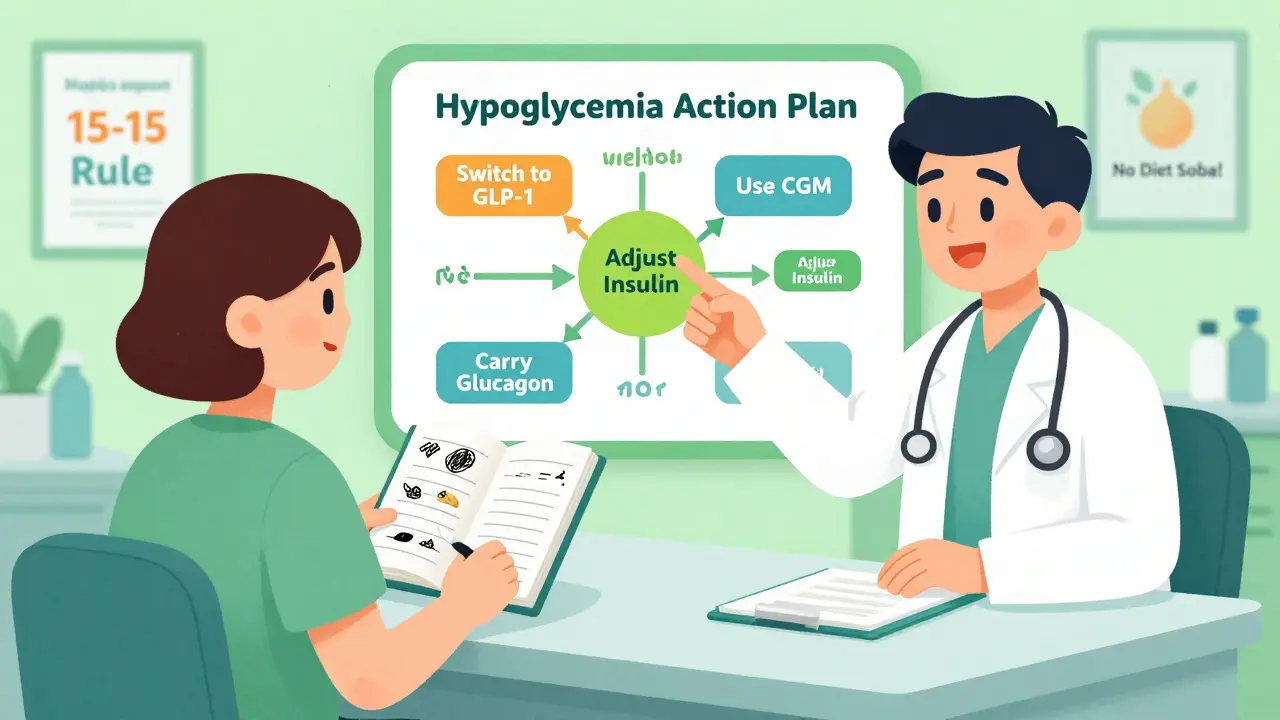
- Use a continuous glucose monitor (CGM). It can alert you if your sugar drops while you sleep.
CGMs reduce severe nighttime lows by 48% compared to fingersticks. But they cost money. Dexcom G7 runs about $399 every 3 months. Freestyle Libre 3 is $89 per month. Medicare now covers CGMs for all insulin users, but out-of-pocket costs still block access for 35% of low-income patients.

Adjust Your Medications-Don’t Just Live With It
If you’re having frequent lows, don’t assume it’s your fault. Talk to your doctor about switching or adjusting meds.Here are proven options:
- Switch from glyburide to glimepiride-second-gen sulfonylureas have 20%-30% fewer lows.
- Use rapid-acting insulin analogs (lispro, aspart) instead of regular insulin-they reduce lows by 19%.
- Consider switching from insulin to a GLP-1 agonist if you’re overweight and your A1C is high enough.
- If you’re on a sulfonylurea and still getting lows, ask about reducing the dose or switching to a non-insulin secretagogue.
Insulin pumps with automated features (like Tandem’s Control-IQ) can reduce nighttime lows by 3.1 hours per night. But they cost $6,500 a year. Not everyone can afford them-but your doctor might help you get insurance coverage.
Track Your Patterns-It’s Not Just About Numbers
You can’t fix what you don’t measure. Logging your blood sugar, meals, activity, and medication timing reveals hidden triggers.One study found patients who kept detailed logs for six weeks reduced hypoglycemia by 52%. But only 28% kept logging beyond six weeks. Why? It feels like a chore.
Make it easier:
- Use your phone’s health app or a free app like Glooko or MySugr.
- Record: time, glucose number, what you ate, insulin dose, activity, and how you felt.
- Look for patterns: Do you always go low after walking the dog? After skipping lunch? After drinking coffee?
Don’t rely on A1C alone. A1C tells you your average-but it hides dangerous dips. One study found 40% of people with “good” A1C levels still had frequent, unnoticed lows.
Carry Emergency Glucagon-And Make Sure Others Know How to Use It
If you pass out from a low, you need someone to give you glucagon. Traditional kits require mixing powder and injecting it-takes 3 minutes. Too slow in an emergency.Now there’s better stuff:
- Baqsimi: Nasal powder. One puff. No needle. $250.
- Gvoke: Prefilled syringe. Easy to use. $350.
- Zegalogue: Liquid glucagon. Ready to inject in 10 seconds. $300.
Keep one in your purse, car, desk, and gym bag. Teach your partner, kids, coworkers-anyone who spends time with you-how to use it. Practice with a trainer kit (many pharmacies give them for free).
Avoid These Common Triggers
Some habits make lows worse. Here’s what to watch for:- Alcohol: Especially on an empty stomach. Causes 22% of severe lows in people under 40.
- Exercise: Without carb adjustments, it causes 31% of daytime lows in active people. Eat 15g carbs before or during long workouts.
- Beta-blockers: Used for high blood pressure or heart issues. They hide the shaking and fast heartbeat-so you don’t feel the low coming. If you’re on one, your doctor needs to know.
- Skipping meals: 68% of people on diabetes forums admit they skip meals to avoid highs. That’s a recipe for lows.
Get Educated-It’s Not Optional
The American Diabetes Association’s “Hypoglycemia Uncovered” program cuts low episodes by 45% in six months. But you have to do it right.Ask your doctor for:
- A personalized hypoglycemia plan
- Training on carb counting (not “servings”-exact grams)
- A review of your insulin-to-carb ratio and correction factor
- A referral to a diabetes educator
It takes 3-5 sessions to learn accurate carb counting. But once you do, you’ll avoid both highs and lows. And you’ll feel more in control.
What to Do If You Keep Getting Lows
If you’ve tried everything and still have frequent hypoglycemia:- Ask for a CGM if you don’t have one.
- Request a review of your insulin regimen-your doses may be too high.
- Check for kidney problems. If your eGFR is below 60, your insulin may build up in your system.
- Ask about switching to a non-insulin medication if your A1C allows it.
- See a diabetes specialist if your primary care doctor isn’t experienced with insulin adjustments.
Hypoglycemia isn’t normal. It’s a sign your treatment plan needs tweaking-not that you’re failing. You’re not alone. And you don’t have to live with it.
What should I do if I feel a low blood sugar coming on but can’t test my glucose?
Treat it as if it’s low. Take 15 grams of fast-acting carbs-glucose tablets, juice, or honey-right away. Don’t wait to test. If you’re unsure, it’s safer to treat and recheck later. Mistreating a low is far riskier than treating a false alarm.
Can I use diet soda or sugar-free candy to treat a low?
No. Diet soda, sugar-free candy, and artificial sweeteners don’t raise blood sugar. They contain no glucose or simple carbs. Only real sugar or pure glucose works fast enough. Using these delays recovery and can lead to a more severe low.
Why do I get low blood sugar after exercising, even when I eat?
Exercise makes your muscles use glucose faster-and keeps them hungry for hours after. Even if you eat before, your body may still pull glucose from your liver. To prevent this, eat 15-30 grams of carbs during longer workouts (over 30 minutes) and reduce your insulin dose by 10%-20% if you’re on insulin. Check your blood sugar before, during, and after.
Is it safe to drive if I have hypoglycemia unawareness?
It’s risky. If you don’t feel your lows, you could pass out behind the wheel. If you have hypoglycemia unawareness, always check your blood sugar before driving. Carry fast-acting carbs in the car. Consider using a CGM with alerts. If you’ve had a severe low in the past 6 months, talk to your doctor about restrictions or whether you should avoid driving until your awareness improves.
How often should I check my blood sugar if I’m on insulin?
At minimum, check before meals, at bedtime, and anytime you feel symptoms. If you’re on multiple daily injections or have frequent lows, check 6-8 times a day. If you use a CGM, you’ll get continuous data-but still check with a fingerstick if the reading doesn’t match how you feel. Consistency is key.


Josh Potter
15 December / 2025Bro this post is a GODSEND. I was almost in the ER last month because I thought a diet soda would save me. Turns out? No. Just no. Glucose tabs in my wallet now. Always. Thanks for not sugarcoating it (pun intended).