Medication Switching Decision Aid Calculator
Compare Your Medication Options
Your Personalized Comparison
| Option A | Option B |
|---|
Visual Risk Comparison
Switching medications isn’t just a doctor’s call-it’s a personal decision that affects your daily life, your body, and your peace of mind. Too often, patients are handed a new prescription without fully understanding why the change is being made, or what they might lose-or gain-by switching. That’s where decision aids come in. These aren’t fancy apps or gimmicks. They’re structured tools designed to help you and your provider weigh the real risks and benefits of changing your meds, especially when side effects are making life harder.
Why Switching Medications Is So Hard
Think about it: you’ve been on a medication for months or years. It works, mostly. But now you’re gaining weight, feeling dizzy, or having trouble sleeping. Your doctor says, "Let’s try something else." But what’s the alternative? Will it be better? Worse? What if the new one causes a side effect you can’t live with?
Studies show that between 25% and 50% of people stop taking their meds within the first year-not because they’re noncompliant, but because they didn’t feel heard. They didn’t understand the trade-offs. One patient switched from warfarin to a DOAC because her doctor said it was "easier," but she didn’t realize the bleeding risk was still there-just different. She ended up in the ER after a fall. Another patient held off on switching antidepressants after seeing an icon array that showed 10 out of 100 people on the new drug got severe nausea. She said, "That’s 10 too many. I’ll stick with what I have."
Decision aids make these numbers real. They turn vague fears into clear choices.
What a Decision Aid Actually Looks Like
A good medication switching decision aid doesn’t just list pros and cons. It shows you what those pros and cons mean in your life.
For example, if you’re considering switching from metformin to an SGLT2 inhibitor for diabetes, the aid might show:
- **Benefit**: 15% lower risk of heart failure over 5 years
- **Risk**: 12% chance of yeast infections (compared to 3% on metformin)
- **Cost**: $300/month vs. $10/month generic
- **Dosing**: Once daily vs. twice daily
But it doesn’t stop there. It uses visual tools-like icon arrays-to show you what those percentages mean. Instead of saying "12% chance," it shows 100 little people. Twelve of them are colored red to represent yeast infections. You see it. You feel it. That’s not abstract. That’s your body.
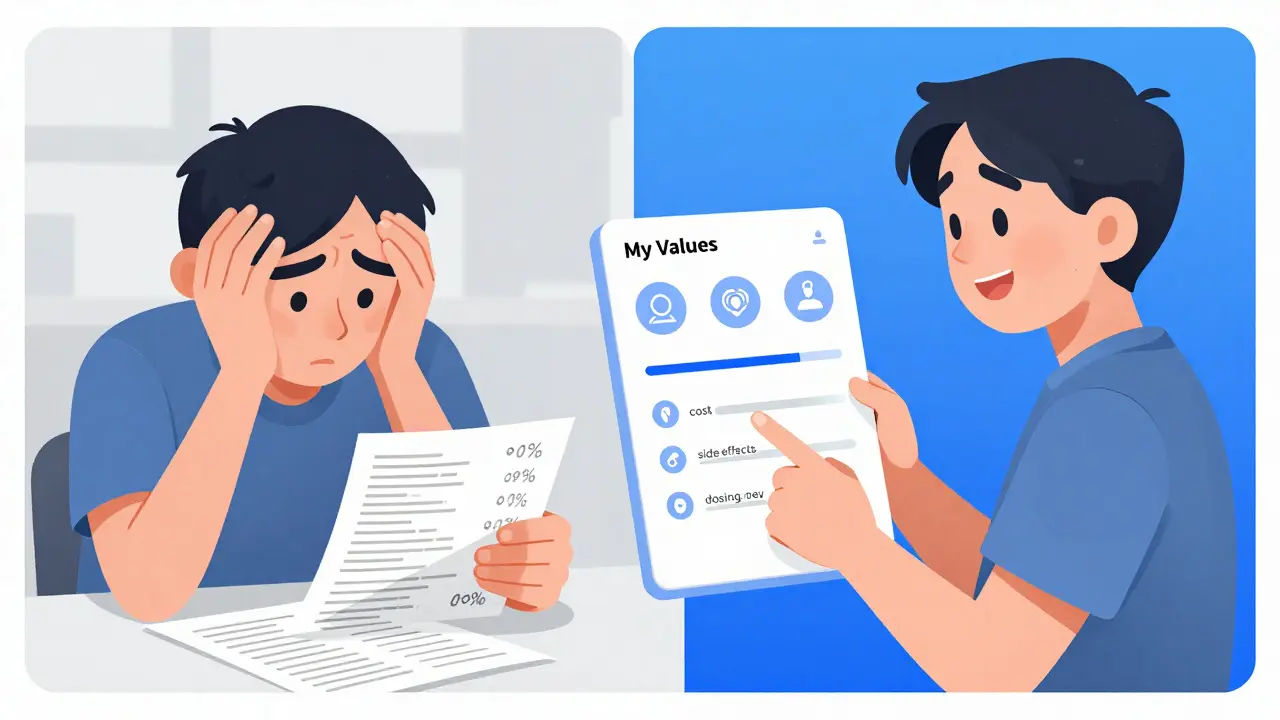
Some tools ask you to rank what matters most: Is cost more important than side effects? Do you hate taking pills twice a day? Do you fear weight gain more than fatigue? Your answers shape the recommendation. This isn’t about what the doctor thinks is best. It’s about what’s best for you.
How Decision Aids Beat Old-School Counseling
Traditional advice sounds like: "This drug works better. It’s proven." But that doesn’t help if you’re terrified of a side effect that’s rare-but terrifying to you.
Research from the Cochrane Collaboration shows patients who use decision aids remember 15-25% more about their options than those who just get a pamphlet. They also feel less stressed about the choice. One 2022 study found decision aids cut decisional conflict by nearly a third.
Why? Because they force you to think about trade-offs. A VA decision aid for blood thinners doesn’t just say, "DOACs are safer." It asks: "If you had a 3% chance of a serious bleed each year, would you still choose this over a 6% chance with warfarin?" It makes you pick a side.
Generic brochures tell you what to do. Decision aids help you decide for yourself.
When Decision Aids Don’t Work
They’re not magic. And they’re not for everyone.
They fall short in emergencies. If you’re having a stroke and need to switch blood thinners right now, there’s no time for icons and rankings.
They also struggle with patients who have severe cognitive issues. A 2022 study found no benefit for people with MMSE scores below 24-meaning they couldn’t process the numbers even with visuals.
And there’s another problem: information overload. One Mayo Clinic study found 31% of users felt overwhelmed by too many stats. If you’re already anxious about your health, seeing 10 different side effect rates can feel like being drowned in data.
Some patients also misinterpret the numbers. One person told her doctor she was "cured" of heart attack risk because the aid said the new drug reduced risk by 22%. She didn’t realize that meant going from a 10% chance to 7.8%-not zero.
That’s why decision aids need a provider nearby. They’re not meant to replace the conversation. They’re meant to make it better.
Real Stories: What Patients Say
On Reddit, a veteran named u/VetMedSurvivor wrote: "The icon array showing 100 people with 3 bleeding events on DOACs versus 8 on warfarin made it real for me." He switched-and hasn’t looked back.
Another patient declined a switch to a new antidepressant after the decision aid showed a 20% chance of sexual side effects. She’d been on her current med for years. The side effects were annoying, but she knew how to manage them. The new one? She didn’t want to risk losing intimacy with her partner.
But not all stories are positive. Some patients felt the tools made different drugs look too similar. One person switched from a statin to a newer cholesterol drug because the aid made both seem equally valid. Later, she found out the newer drug had only been tested for 2 years, while the statin had 30 years of data. She felt misled.
That’s why transparency matters. The best decision aids don’t hide uncertainty. They say: "We don’t know everything yet. Here’s what we do know."
How to Use a Decision Aid-Step by Step
If your provider offers one, here’s how to get the most out of it:
- Ask for it early. Don’t wait until the day of your appointment. Request the aid 24-72 hours before your visit. Give yourself time to read it, sit with it, and write down questions.
- Use it alone first. Don’t let your provider rush you through it. Take notes on what surprises you, what scares you, what you don’t understand.
- Bring your list. Say: "I saw that this drug has a 15% chance of weight gain. That’s a dealbreaker for me. Is there another option?"
- Ask for clarification. If you see a percentage, ask: "Is that 15 out of 100 people? Or 15 out of 1,000?" Numbers mean nothing without context.
- Don’t feel pressured. You don’t have to decide in the room. Say: "I need a day to think about this."
Some tools are built into patient portals like MyChart or Epic. Others are standalone websites. The VA’s MIRECC program and the Ottawa Hospital Research Institute both offer free, publicly available aids for common switches like anticoagulants, diabetes meds, and antidepressants.
What’s Changing in 2025
Decision aids are getting smarter. In early 2024, Intermountain Healthcare launched an AI-powered tool that adjusts how risks are shown based on how you learn. If you respond better to pictures, it shows more icons. If you prefer words, it gives you more narrative. If you skip ahead, it flags that you might be missing key info.
The FDA is also stepping in. In 2024, they proposed new rules requiring decision aids to be tested on diverse patient groups-including those with low literacy or limited English-to make sure they’re truly understandable.
Medicare now ties quality bonuses to shared decision-making. That means more clinics will be required to offer these tools. But here’s the catch: only 38% of hospitals have money set aside to update them. Medications change fast. A decision aid that’s accurate today might be outdated in 18 months.
Who Should Use These Tools?
Decision aids work best for "preference-sensitive" decisions-where more than one option is medically valid, and the choice depends on your values.
Examples:
- Switching from warfarin to a DOAC for atrial fibrillation
- Choosing between GLP-1 agonists for type 2 diabetes
- Switching antidepressants after side effects
- Deciding whether to switch from a statin to a newer cholesterol drug
They’re less useful for clear-cut cases-like switching from one antibiotic to another when the first didn’t work. There, the evidence is straightforward. No need for icons.
What to Do If Your Doctor Doesn’t Offer One
You don’t need to wait for permission. Ask: "Is there a decision aid I can look at before we decide on a new medication?"
Here are three trusted sources you can use right now:
- Mayo Clinic Decision Aids - Covers diabetes, heart disease, mental health
- VA MIRECC - Free, evidence-based tools for veterans and the public
- Ottawa Hospital Research Institute - 42+ tools, available in 12 languages
Print them. Read them. Bring them to your next visit. You’re not being difficult-you’re being smart.
The Bottom Line
Switching medications should never be a gamble. You shouldn’t have to guess whether a new drug will make you feel better-or worse. Decision aids give you back control. They turn confusion into clarity. They turn fear into informed choice.
Yes, they take time. Yes, they’re not perfect. But when used right, they’re the closest thing we have to a fairness tool in medicine. They ensure your voice isn’t lost in the noise of clinical guidelines and insurance formularies.
If you’re thinking about switching meds-especially because of side effects-don’t just nod along. Ask for the numbers. Ask for the pictures. Ask for the choices. Your body deserves nothing less.
What is a medication switching decision aid?
A medication switching decision aid is a structured tool-usually digital-that helps patients and providers make informed choices when considering a change in medication. It presents balanced information on the benefits, risks, and side effects of current and alternative treatments, often using visuals like icon arrays and comparative tables. It also includes interactive exercises to help patients clarify what matters most to them, such as cost, dosing frequency, or specific side effects.
Are decision aids only for complex medications?
No, but they’re most valuable when there’s no single "best" option. They work best for preference-sensitive decisions-like switching antidepressants, blood thinners, or diabetes meds-where multiple treatments are equally effective, but the side effect profiles differ. For simple cases, like switching from one antibiotic to another after failure, they’re usually unnecessary.
Can I use a decision aid on my own, or do I need my doctor?
You can use one on your own to get informed, but the full benefit comes from using it with your provider. Decision aids are designed to spark a conversation-not replace it. Your doctor helps interpret the numbers, explain uncertainties, and match your values to realistic options. Using it alone helps you prepare; using it together helps you decide.
Do decision aids work for older adults or people with cognitive issues?
They can, but not always. Studies show decision aids are less effective for patients with cognitive impairment, especially those with MMSE scores below 24. In these cases, simplified visuals, verbal explanations, and caregiver involvement are needed. Some tools now offer audio versions or simplified layouts, but they’re not a substitute for personalized support in complex cases.
Are decision aids free to use?
Yes, most high-quality decision aids are free and publicly available. Sources like the Ottawa Hospital Research Institute, the VA’s MIRECC program, and Mayo Clinic offer their tools at no cost. Some commercial platforms exist, but they’re typically used by health systems, not patients directly. Always check the source-stick to academic or government-backed tools for reliable, unbiased information.
What if I don’t like the option the decision aid suggests?
That’s okay. Decision aids don’t tell you what to choose-they show you what your choices mean. If the top recommendation doesn’t feel right, say so. Your values matter more than the tool’s suggestion. Maybe you’re willing to accept more side effects to avoid a certain cost. Maybe you’re terrified of weight gain, even if it’s rare. The tool’s job is to help you say that out loud-and your provider’s job is to honor it.
How often are decision aids updated?
Ideally, every 18 to 24 months, as new drug data emerges or FDA labels change. But many tools lag behind. Only 38% of hospitals have dedicated funding to keep them current. Always check the publication or last update date on the tool. If it’s older than two years, ask your provider if newer evidence exists.
Can decision aids help with side effect management?
Yes, that’s one of their biggest strengths. They help you compare side effect risks across options-not just in percentages, but in real-life terms. If you’re struggling with nausea, fatigue, or sexual side effects, a decision aid lets you see how likely those are with each medication. That way, you can choose the one that aligns with what you can tolerate, not just what’s statistically "better."



Winni Victor
24 December / 2025This whole thing feels like a corporate scam dressed up as patient empowerment. They give you a shiny infographic and call it a 'decision aid'-but the real decision? That’s still made by the insurance company’s formulary. I’ve seen these tools. They always make the expensive new drug look 'equally valid' while quietly burying the 30-year safety data under a pile of pretty icons. Don’t be fooled. They’re not helping you-they’re clearing liability.