Carpal tunnel syndrome isn’t just a tingling hand-it’s a sign your median nerve is being crushed. Every day, millions of people wake up with numb fingers, achy wrists, or a hand that feels like it’s asleep. For many, it starts as a nuisance. For others, it becomes a life-altering condition that makes buttoning a shirt or holding a coffee cup impossible. The truth? This isn’t just "overuse"-it’s a serious nerve compression problem that gets worse the longer you ignore it.
What Exactly Is Carpal Tunnel Syndrome?
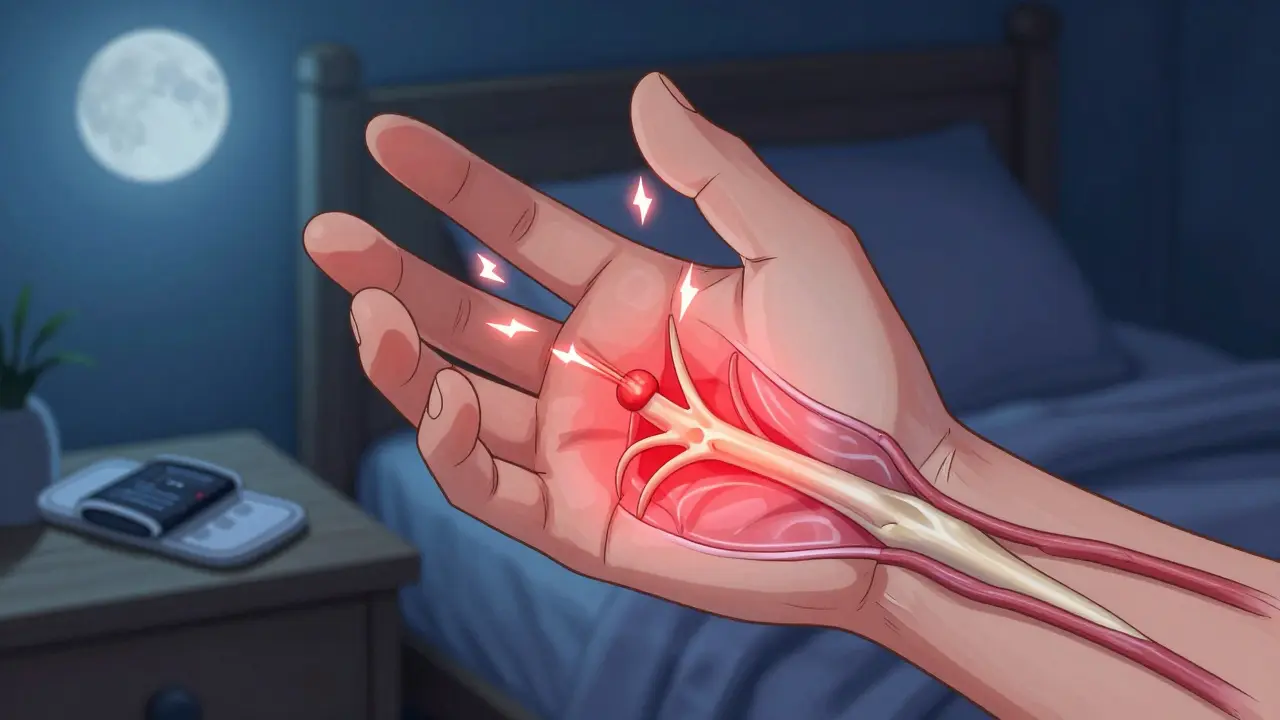
Carpal tunnel syndrome (CTS) happens when the median nerve, which runs from your forearm into your palm, gets squeezed inside a narrow passageway in your wrist called the carpal tunnel. This tunnel isn’t made of muscle or skin-it’s a rigid channel formed by wrist bones on one side and a tough ligament on the other. Inside it, nine tendons bend your fingers, and the median nerve gives feeling to your thumb, index, middle, and half your ring finger.
When pressure builds up in that tunnel-because of swelling, repetitive motion, or even just anatomy-the nerve starts to misfire. You don’t just feel numbness. You feel burning, electric shocks, or a dull ache that climbs up your arm. Symptoms often hit hardest at night, waking you up because your hand feels like it’s on fire. Shaking it helps-briefly. But if you’re still dealing with it in the morning, it’s not just tiredness. It’s progression.
Studies show about 10% of people in the U.S. will develop CTS in their lifetime. Women are three times more likely than men to get it, especially between ages 45 and 60. Why? Hormonal changes, smaller carpal tunnels, and higher rates of jobs involving repetitive hand movements all play a role.
How Do You Know It’s CTS-and Not Something Else?
Not every numb hand is carpal tunnel. Arthritis, neck pinched nerves, or even diabetes can mimic the symptoms. But CTS has a signature pattern:
- Numbness or tingling in the thumb, index, middle, and radial side of the ring finger
- Pain that radiates up the forearm, sometimes to the shoulder
- Symptoms worse at night or after repetitive tasks like typing, gripping tools, or holding a phone
- Weakness in your grip-dropping things, struggling to open jars
Doctors use a few simple tests to confirm it. The Phalen test? Hold your wrists bent forward for a minute. If your fingers tingle, that’s a red flag. The Tinel sign? Tap gently over your wrist. A shock-like feeling in your fingers means the nerve is irritated. Then there’s the carpal compression test-pressing directly on the tunnel for 30 seconds. If symptoms flare, it’s likely CTS.
For unclear cases, doctors turn to nerve conduction studies. These measure how fast electrical signals move through the median nerve. If it’s slower than 3.7 milliseconds across the wrist, that’s diagnostic. But here’s the catch: about 15-20% of people over 60 show abnormal nerve tests even when they have no symptoms. That’s why clinical signs matter more than test numbers alone.
The Three Stages of Carpal Tunnel Syndrome
CTS doesn’t hit all at once. It creeps in. And it progresses in clear stages:
- Mild: Symptoms come and go-mostly at night. You wake up shaking your hand. No weakness. No permanent numbness. This stage is often dismissed as "just sleeping funny."
- Moderate: Symptoms start showing up during the day. Typing, driving, or holding a book triggers tingling. You begin avoiding certain tasks. Nighttime symptoms get worse. You might start noticing your grip isn’t as strong.
- Severe: Numbness is constant. Muscles at the base of your thumb start to waste away. You can’t pick up small objects. Buttoning clothes becomes a chore. This is when nerve damage becomes permanent.
Once muscle atrophy shows up, you’re past the point where splints or injections alone can fix things. The nerve’s already been damaged too long. That’s why early action matters.

Conservative Treatments That Actually Work
If you’re in the mild or moderate stage, you have options-real ones that work for most people.
Wrist splints at night are the gold standard. Not just any brace-properly fitted ones that hold your wrist in a neutral position (not bent up or down). Studies show 60-70% of people see major improvement after 4-6 weeks of consistent use. The key? Wear it every night. No exceptions. If you skip nights, you’re resetting the clock.
Nerve gliding exercises help too. These aren’t stretches for your muscles-they’re gentle movements that help the nerve slide smoothly through the tunnel. A physical therapist can teach you these in 2-4 sessions. Do them daily. They reduce swelling and prevent the nerve from sticking.
Corticosteroid injections give quick relief. About 70% of patients feel better for 3-6 months. But they’re not a cure. They reduce inflammation around the nerve, buying you time. If your symptoms have lasted over a year, injections are less likely to help. One study found only a 35% success rate for those with symptoms longer than 12 months.
Activity changes are non-negotiable. Avoid bending your wrist more than 30 degrees. That means adjusting your keyboard height, switching from a mouse to a trackball, or taking breaks every 20 minutes. If you work in healthcare, manufacturing, or food service-industries with the highest CTS rates-you need ergonomic tweaks, not just willpower.
Cost-wise, conservative care runs $450-$750 in the U.S. That includes splints ($150-$250), physical therapy ($100-$200 per session), and one injection ($300-$500). It’s cheaper than surgery-and far less risky.
Surgery: When It’s Time to Cut
If you’ve tried splints, exercises, and injections for 6-8 weeks with no improvement-or if you have muscle loss-you need surgery. The goal? Cut the ligament pressing on the nerve. That’s it. No nerves are removed. No bones are broken. Just enough pressure is released so the nerve can heal.
There are two main types:
- Open release: A 2-inch cut along the palm. The ligament is cut directly. Recovery takes 6-8 weeks for full strength.
- Endoscopic release: One or two tiny cuts. A camera guides a small tool to cut the ligament from inside. Recovery is faster-often 2-3 weeks sooner.
Success rates? 90-95%. Most people regain full function. But it’s not perfect. About 15-30% get "pillar pain"-tenderness on the sides of the palm. Scar tenderness happens in 5-10%. Nerve injury? Rare-under 1%.
Recent advances include ultrasound-guided procedures like the Sonex Health MicroKnife. Approved by the FDA in 2021, it’s done through a needle-sized incision. Patients report 40% less pain and return to work 50% faster than with traditional surgery.
Out-of-pocket cost? $1,200-$2,500 with insurance. Endoscopic is 15-20% more expensive but cuts recovery time. Physical therapy after surgery? Usually 6-8 sessions over 4-6 weeks. Light work? Back in 2-3 weeks. Heavy lifting? Wait 10-12 weeks.

What Doesn’t Work (And Why)
There’s a lot of noise out there. Yoga? Some studies show mild benefit, but not enough to replace proven methods. Acupuncture? No strong evidence. Anti-inflammatory diets? Helpful for general health, but won’t un-squeeze a nerve. Vitamin B6? No reliable data supports it for CTS.
And don’t fall for "carpal tunnel bracelets" or magnetic wristbands. They don’t reduce pressure. They don’t change nerve function. They’re expensive placebo devices.
The biggest mistake? Waiting. The longer you wait, the less likely conservative care will work. A 2023 review in JAMA Neurology found people who started splinting and exercises early were 45% less likely to need surgery within two years.
Prevention and Long-Term Outlook
CTS isn’t inevitable. You can reduce your risk:
- Keep your wrists straight while typing or using tools
- Take short breaks every 20 minutes to stretch your fingers and shake out your hands
- Use ergonomic keyboards, mice, and tools
- Manage conditions like diabetes or thyroid disease-they increase nerve vulnerability
Even if you’ve had CTS before, proper habits can prevent recurrence. Workers in high-risk jobs should push for workplace assessments. In the EU, this is required. In the U.S.? Not yet. But that doesn’t mean you can’t ask.
Projections show CTS cases will rise 12% over the next decade. More screen time, more repetitive tasks, an aging population-it’s a perfect storm. But awareness is growing. Ultrasound is now recommended as a first-line diagnostic tool in many clinics. Treatment is becoming faster, less invasive, and more precise.
The bottom line? Don’t wait for your hand to stop working. If you’ve had symptoms for more than a few weeks, see a doctor. Get diagnosed. Start treatment. Your future self will thank you.
Can carpal tunnel syndrome go away on its own?
Rarely. Mild symptoms might improve with rest and wrist positioning, but without addressing the root cause-nerve compression-the problem will return and likely worsen. Waiting for it to "fix itself" often leads to permanent nerve damage. Early intervention is key.
Is carpal tunnel syndrome caused by typing?
Not directly. Typing alone doesn’t cause CTS. But repetitive wrist flexion, forceful gripping, or working with your wrists bent for long periods-common in typing, assembly work, or using hand tools-can trigger swelling that compresses the nerve. It’s the combination of motion, pressure, and poor ergonomics, not typing itself.
How long does it take to recover from carpal tunnel surgery?
Most people return to light duties in 2-3 weeks. Full recovery takes 6-8 weeks. Endoscopic surgery may shorten this by 2-3 weeks. Manual laborers often need 10-12 weeks. Pain and swelling peak in the first week, then gradually improve. Physical therapy helps restore strength and flexibility.
Are wrist splints really effective for carpal tunnel?
Yes-if used correctly. Nighttime splinting that holds the wrist in a neutral position improves symptoms in 60-70% of mild to moderate cases. The key is consistency: wear it every night for at least 4-6 weeks. Wearing it only sometimes won’t help. Custom-fitted splints work better than cheap ones.
Can carpal tunnel come back after surgery?
It’s uncommon, but possible. If the ligament regrows or scar tissue forms around the nerve, symptoms can return. This happens in less than 5% of cases. More often, recurrence is due to new injuries or failure to change aggravating habits. Proper ergonomics and activity modification after surgery greatly reduce the risk.
What’s the difference between carpal tunnel and tendonitis?
Tendonitis is inflammation of the tendons-often causing pain during movement. Carpal tunnel is nerve compression-causing numbness, tingling, and weakness. Tendonitis hurts when you move your wrist. CTS makes your fingers feel asleep. They can happen together, but the treatments differ. Tendonitis responds to rest and anti-inflammatories. CTS needs pressure relief-splints, injections, or surgery.
If you’ve been ignoring tingling hands, now’s the time to act. Carpal tunnel syndrome doesn’t get better with time-it gets worse. But with the right approach, you can stop it before it steals your grip, your sleep, or your independence.

Jay Ara
25 December / 2025been dealing with this for months just thought it was stress. started wearing a splint last week and honestly my fingers dont feel like theyre on fire anymore. no magic just consistency.