When you're managing bipolar disorder with lithium carbonate, the brand on the bottle matters more than most people realize. It's not just about cost - it's about your blood levels, your safety, and whether the medicine actually works. Even though generic lithium carbonate is approved as bioequivalent to brand-name versions, lithium carbonate generics can behave differently in your body. And when you're dealing with a drug that has a razor-thin line between healing and harm, that difference can be dangerous.
Why Lithium Is So Tricky
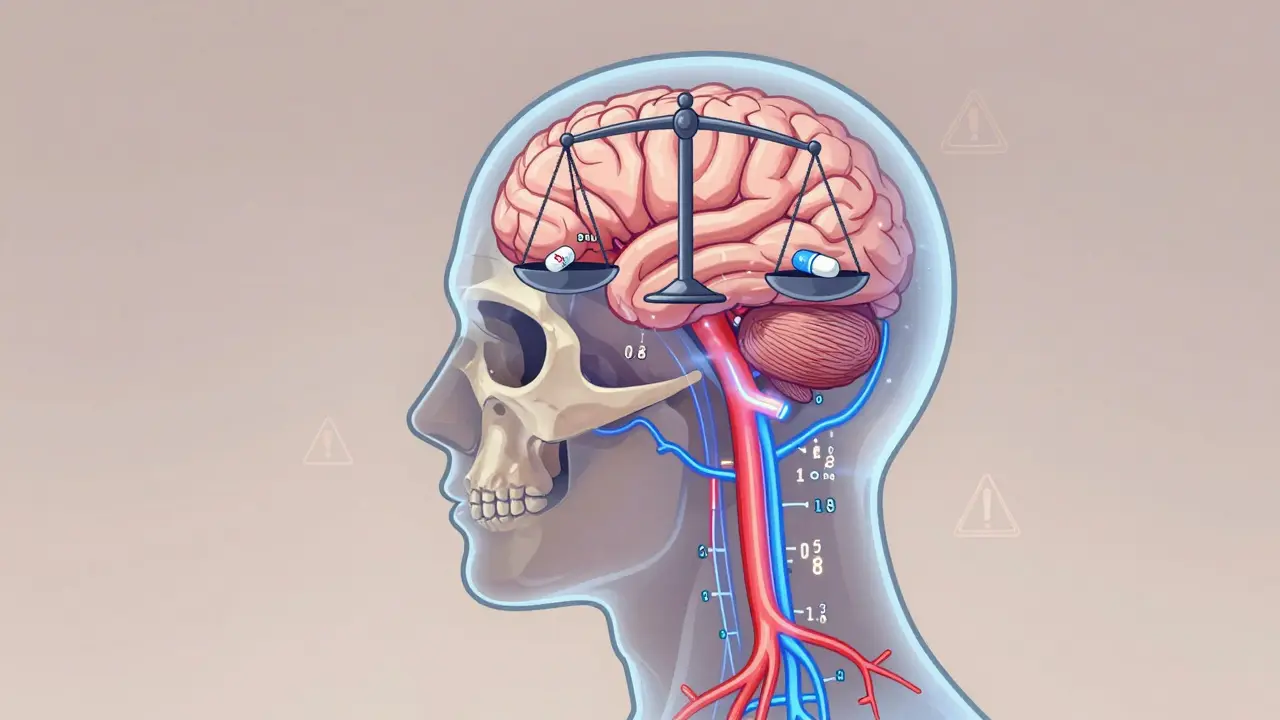
Lithium isn't like most medications. You can't just take a pill and assume it's working. It has a narrow therapeutic index, meaning the dose that helps you stay stable is almost the same dose that can poison you. The safe range? Between 0.6 and 1.2 mmol/L. Go above 1.5 mmol/L, and you risk tremors, confusion, or worse - seizures, heart rhythm problems, even coma. Below 0.6 mmol/L, and you might not feel any benefit at all.This isn't theoretical. In 1981, a landmark study by Baastrup and Schou showed that lithium cuts relapse rates in bipolar disorder by more than half. But that only works if your levels are in the right zone. And here's the catch: two pills that look identical, one branded, one generic, might not release lithium the same way in your bloodstream.
Formulation Differences That Matter
Not all lithium carbonate is made the same. There are two main types: immediate-release and sustained-release (also called extended-release or controlled-release). Immediate-release versions hit peak levels in your blood within 1 to 2 hours. Sustained-release versions, like Priadel or Camcolit, take 4 to 5 hours to reach their peak. That might sound minor, but it changes how your body handles the drug - and how you monitor it.For immediate-release lithium, doctors draw your blood 12 hours after your last dose. For sustained-release, they often wait 24 hours. If you switch from one type to another without adjusting your monitoring schedule, you could get a misleading result. A level that looks normal might actually be dangerously high - or too low - because the timing was off.
A 2024 study in the Journal of Psychopharmacology found something startling: when patients switched from Priadel to Camcolit - both sustained-release - their average serum levels went up by 11%, even when the dose stayed the same. That’s not a small fluctuation. That’s the difference between a safe level and a toxic one. And in four patients in that study, switching brands pushed their levels above 1.3 mmol/L - one even hit 1.88 mmol/L, which is in the danger zone.
Generics Aren’t Always Interchangeable
The FDA says generics must be within 80-125% of the brand’s absorption rate to be approved. That sounds precise - until you realize lithium’s therapeutic window is only 0.6 mmol/L wide. A 25% variation in absorption could mean the difference between 0.7 mmol/L and 0.9 mmol/L - or worse, between 0.9 mmol/L and 1.1 mmol/L. Both are technically "therapeutic," but one might cause side effects while the other doesn’t.Studies from the 1980s already showed up to 20% variation in peak levels between different sustained-release formulations. Fast forward to today, and we still don’t have a reliable way to predict how a new generic will behave in your body. Even if the pill contains the same amount of lithium carbonate, the fillers, coatings, and manufacturing processes can change how fast or how completely it dissolves.
That’s why experts now warn against automatic generic substitution without checking your blood levels after the switch. If your pharmacist swaps your Priadel for a cheaper generic without telling you, and your doctor doesn’t retest your serum lithium, you could be walking into a risk you never saw coming.

Target Levels Aren’t One-Size-Fits-All
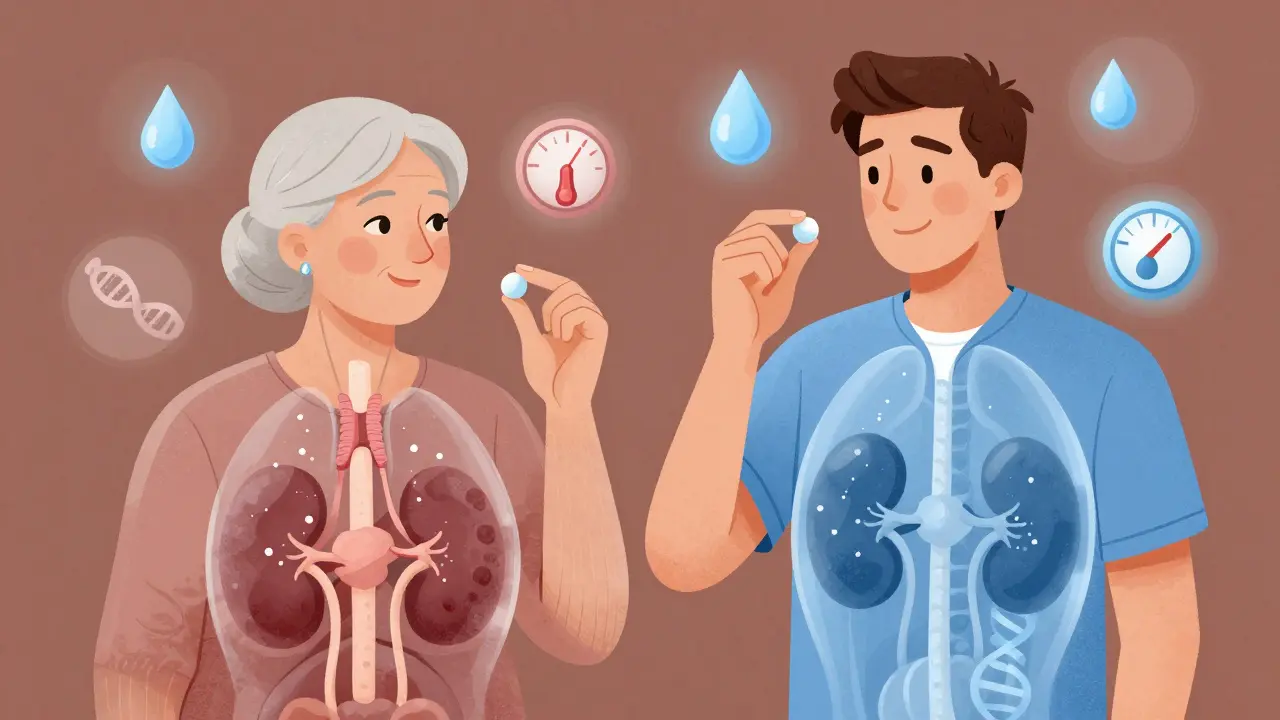
There’s no single "correct" lithium level for everyone. The American Psychiatric Association recommends 0.8-1.0 mmol/L for acute episodes and 0.6-0.8 mmol/L for long-term maintenance. But even that’s not set in stone.For older adults - especially those over 60 - many clinicians lower the target by 20-25%. Why? Because kidney function declines with age, and lithium is cleared mostly through the kidneys. A level that’s safe for a 30-year-old might be toxic for an 80-year-old. One study found patients over 80 received, on average, 437 mg less lithium per day than those under 30 - not because they needed less, but because their bodies couldn’t handle the same dose.
Women also tend to need lower doses than men - about 96 mg less on average - even after adjusting for weight and other factors. Hormonal differences, body composition, and kidney clearance all play a role. And if you have thyroid problems - which happens in up to 15% of people on long-term lithium - your dose may need adjustment too.
Monitoring Is Non-Negotiable
If you're on lithium, you need regular blood tests. No exceptions. During dose changes, you should be tested every week or two. Once you’re stable, every 3 to 6 months is the minimum. But here’s what many people don’t realize: it’s not just about lithium levels.You also need to check your kidney function - not just creatinine, but eGFR-cystatin C, which is more accurate for detecting early kidney damage. Thyroid levels too. Lithium can cause hypothyroidism, which mimics depression. If your TSH is high and you’re feeling sluggish, it might not be your bipolar disorder - it might be your thyroid.
And don’t forget hydration. Dehydration - from a fever, diarrhea, or even just drinking less water - can spike your lithium levels. That’s why doctors tell you to keep drinking fluids, especially in hot weather. In Darwin, where summer temperatures regularly hit 35°C, this isn’t just advice - it’s survival.
What Happens When You Switch Brands
Let’s say your doctor switches you from a brand-name lithium to a generic because of cost. You feel fine. You don’t tell anyone. Three months later, you’re more irritable, your hands are shaking, and you’re nauseous. Your doctor assumes it’s a mood episode - but it’s not. It’s lithium toxicity.That scenario happened in the 2024 study. Four patients had serum levels above 1.3 mmol/L after switching generics. None of them had their levels checked after the switch. All four were misdiagnosed - until someone finally ran the test.
The takeaway? Any time you change lithium formulations - even if it’s just a different generic - get your serum level checked within 1-2 weeks. Don’t wait for symptoms. Don’t assume it’s the same. Lithium doesn’t care what the label says. It only cares what’s in your blood.
What’s Changing Now
The FDA is starting to catch up. In 2023, they issued draft guidance requiring pharmacokinetic studies for modified-release lithium generics - not just bioequivalence tests. That’s a big deal. It means future generics will have to prove they behave like the original in real people, not just in test tubes.Meanwhile, researchers are exploring genetic markers that predict how someone metabolizes lithium. The International Consortium on Lithium Genetics has found 30 genes linked to lithium response and clearance. In the next few years, we may see personalized dosing tools - apps or AI systems that use your age, weight, kidney function, and genetic profile to recommend your ideal dose.
But for now, the best tool we have is still the blood test. Simple. Cheap. Reliable.
Final Advice: Know Your Numbers
Lithium is one of the oldest and most effective mood stabilizers we have. It reduces suicide risk by up to 80% in people with bipolar disorder. But it’s not a drug you can take on autopilot.If you’re on a generic lithium carbonate, know which one you’re taking. Keep a list of the brand names and manufacturers. If your pharmacy switches it, ask your doctor to retest your serum level. Don’t wait. Don’t assume. Your brain depends on it.
And if you’re a clinician - don’t just prescribe. Monitor. Educate. Track. Lithium doesn’t fail patients. Inconsistent monitoring does.
Can I switch between lithium carbonate generics without checking my blood levels?
No. Even though generics are required to be bioequivalent, real-world studies show significant differences in serum levels after switching brands. Always check your lithium level 1-2 weeks after any formulation change - whether it’s a different generic or a switch from brand to generic.
What’s the safest lithium serum level for long-term use?
For most adults in maintenance phase, 0.6-0.8 mmol/L is considered safest. Some clinicians target 0.8-1.0 mmol/L for better mood control, but this increases side effect risk. For people over 60, aim for 0.4-0.7 mmol/L due to reduced kidney clearance. Always follow your doctor’s guidance based on your individual needs.
Why do some people need higher doses than others on the same generic?
Lithium dosing varies due to age, weight, kidney function, thyroid status, hydration, and even genetics. A 25-year-old man with strong kidneys may need 1200 mg daily, while a 70-year-old woman with mild kidney decline may need only 600 mg. Your body’s ability to clear lithium determines your dose - not your weight alone.
Do I need to avoid salt or caffeine while on lithium?
You don’t need to avoid salt or caffeine entirely, but you must keep your intake consistent. Sudden drops in sodium (like on a low-salt diet) can cause lithium levels to rise. Large amounts of caffeine can increase lithium clearance, lowering your levels. Stability - not restriction - is key.
How often should I get my blood tested on lithium?
When starting or adjusting your dose, test every 1-2 weeks. Once stable, every 3-6 months is standard. But if you’re over 60, have kidney or thyroid issues, or live in a hot climate, test every 2-3 months. Also test after any illness, dehydration, or medication change.
Is lithium still used today, or are newer drugs better?
Lithium remains first-line for bipolar I disorder maintenance. Studies show it’s more effective than newer drugs at preventing suicide and long-term relapse. While newer medications have fewer monitoring requirements, none match lithium’s proven track record. About 60% of long-term bipolar patients still take it - and for good reason.
What to Do Next
If you’re on lithium carbonate - generic or brand - here’s your action plan:- Write down the exact name of your current lithium product (e.g., "Camcolit 300 mg").
- Ask your pharmacist if your prescription was filled with the same brand as last time.
- Request a serum lithium level check if you’ve switched brands in the last 30 days.
- Get your kidney and thyroid function tested at least twice a year.
- Keep a log of your symptoms, fluid intake, and any illness or weight changes.
Lithium works - but only if you treat it like the precision tool it is. Not a pill. Not a cure. A delicate balance - and your blood level is the only way to know you’re on it.

Anna Weitz
27 December / 2025Lithium isn't medicine it's a tightrope walk with a poison net below and everyone acts like it's aspirin
you switch generics and suddenly your brain is on fire or frozen and no one checks because it's cheaper
we treat mental health like a spreadsheet not a human body