Lamotrigine-Valproate Dosing Calculator
Dosage Adjustment Calculator
Recommended Dose
This dose should be taken
Titration Schedule
Critical Safety Warning
Stop both medications immediately if you experience:
- Red, blotchy rash anywhere on body
- Blisters or peeling skin
- Fever, sore throat, or swollen glands
- Red eyes or mouth sores
This is a medical emergency - seek immediate help
When you take lamotrigine with valproate, your risk of a serious skin rash goes up - not because the drugs fight each other, but because one changes how your body processes the other. This isn’t just a theoretical concern. In the 1990s, doctors saw a spike in life-threatening rashes like Stevens-Johnson syndrome in patients using both drugs. Many of these cases were preventable. Today, the risk is low - but only if you follow the right dosing rules.
Why This Interaction Happens
Valproate doesn’t make lamotrigine more toxic. Instead, it slows down how fast your liver breaks down lamotrigine. Normally, lamotrigine is cleared from your body through a process called glucuronidation. Valproate blocks that pathway. The result? Lamotrigine builds up in your blood - often doubling or even tripling its concentration. Higher levels mean higher risk of rash.This isn’t a guess. Multiple studies, including data from the German severe cutaneous reaction registry, show a direct link between unadjusted lamotrigine doses and serious skin reactions. After doctors started lowering starting doses and slowing titration, the number of life-threatening rashes dropped dramatically. By 1999, serious cases had fallen to just 3 out of nearly 18,000 exposures.
The Real Danger: How Fast You Increase the Dose
Rash risk isn’t about the final dose. It’s about how quickly you get there. If you start lamotrigine at 50 mg a day while already on valproate, you’re putting yourself at risk. The same dose might be fine if you’re not on valproate - but with it, that 50 mg could be equivalent to 100 mg in your bloodstream.Most rashes appear within the first 8 weeks. They often start as a mild redness or itching, but can quickly turn into blisters, peeling skin, or widespread rashes covering large areas of the body. In rare cases, it can become Stevens-Johnson syndrome or toxic epidermal necrolysis - conditions with mortality rates of 5-35%. These aren’t common, but when they happen, they’re devastating.
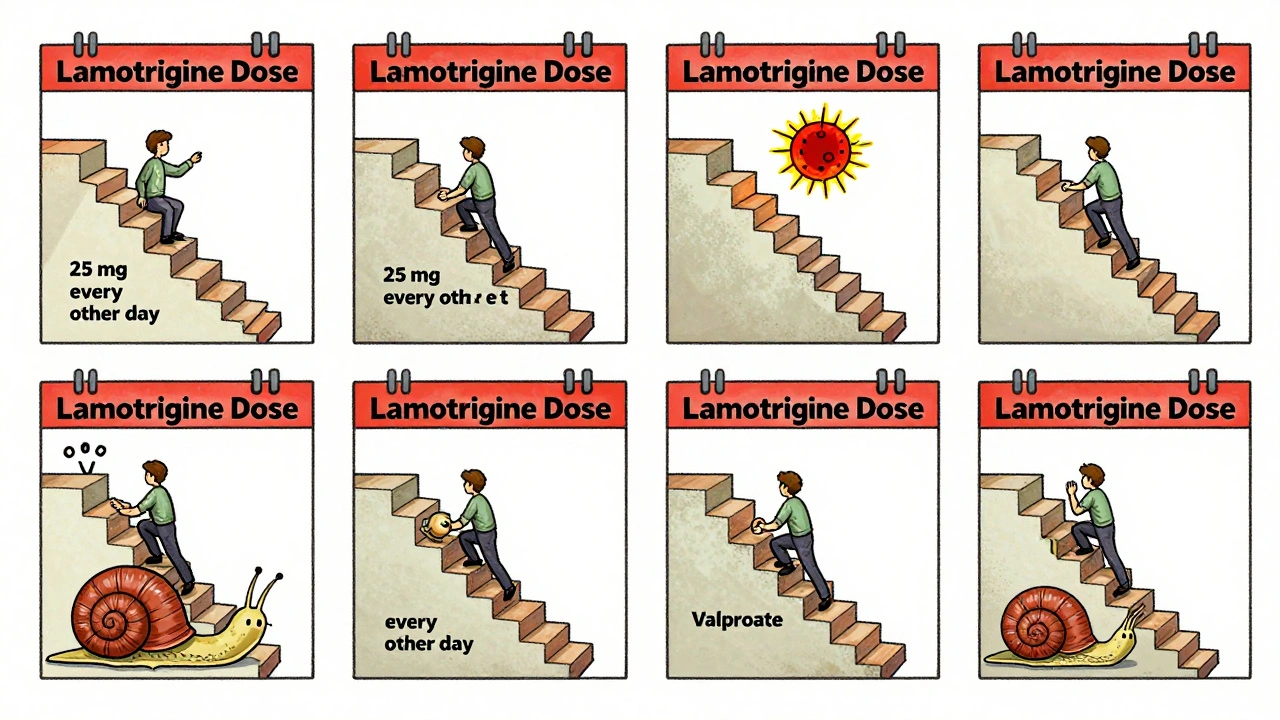
What the Dosing Rules Actually Look Like
If you’re starting lamotrigine while already taking valproate, here’s what works:- Start at 25 mg every other day - not daily.
- Wait two weeks before increasing.
- Then increase by 25 mg every two weeks (e.g., 25 mg daily → 50 mg daily → 75 mg daily).
This is drastically different from the standard lamotrigine titration, which usually starts at 25 mg daily and increases every week. With valproate, you’re moving at half-speed. Many doctors skip this and start at 25 mg daily - a mistake that increases risk.
For children and teens on both drugs, some experts recommend starting even lower: 12.5 mg every other day. That’s because younger patients may be more sensitive to the interaction, and their metabolism can be unpredictable.
What Happens If You Add Valproate to an Existing Lamotrigine Regimen?
This is a common scenario. Someone’s been stable on lamotrigine for months - maybe for bipolar disorder or epilepsy - and now their doctor adds valproate. Do you need to cut the lamotrigine dose?Yes. Even if you’ve been on lamotrigine for a year, adding valproate still cuts its clearance by about half. That means your lamotrigine blood level will rise sharply within days. The risk of rash doesn’t disappear just because you’ve tolerated lamotrigine before.
The rule here is simple: reduce your current lamotrigine dose by 50% when you start valproate. So if you’re on 100 mg daily, drop to 50 mg daily. Then, after two weeks, you can slowly increase back up - but only if no rash appears. Monitor closely. Don’t assume you’re safe just because you’ve been on it for a while.
What Else Can Trigger a Rash?
Valproate and lamotrigine aren’t the only factors. The biggest non-drug predictor of an AED rash? Having had one before. If you’ve ever had a rash from any antiepileptic drug - carbamazepine, phenytoin, even topiramate - your risk of reacting to lamotrigine jumps by over three times.Other factors? Genetics. Some people have variations in liver enzymes that make them slow metabolizers. But right now, we don’t test for those in routine practice. So the only reliable tool is dose control.
One 2023 case report described an 18-year-old with bipolar disorder who developed not just a rash, but swollen lymph nodes and fever - signs of a systemic reaction. Even after stopping lamotrigine, symptoms got worse for three days. She needed steroids to recover. This shows that the reaction isn’t always skin-deep. It can involve your immune system broadly.
What to Do If You Notice a Rash
Don’t wait. Don’t take antihistamines and hope it goes away. If you see:- A red, blotchy rash anywhere on your body
- Blisters or peeling skin
- Fever, sore throat, or swollen glands
- Red eyes or mouth sores
Stop both drugs immediately and call your doctor. Don’t wait for it to get worse. Even if the rash seems mild, it could be the start of something serious. In some cases, stopping the drugs and giving steroids or antihistamines is enough - and the rash clears in days. But delay can mean hospitalization.

Is This Risk Worth It?
Both drugs are powerful. Lamotrigine is one of the most effective mood stabilizers for bipolar disorder. Valproate works well for seizures and mania. Many patients do great on both - especially when dosed correctly.One study of 80 young patients on both drugs found only two rashes - 2.5%. But that study also noted sedation and fatigue were common. The low rash rate likely came from careful dosing. In real-world use, when doctors skip the slow titration, the risk climbs.
Compare that to other antiepileptic drugs. The average rash rate across 15 common AEDs is 2.8%. Lamotrigine alone carries a higher baseline risk - but with valproate, it’s even higher. The difference between 0.13% and 2.8% is huge. That’s why the dosing rules exist.
What’s Changed Since the 1990s?
Back then, lamotrigine was introduced with a standard titration schedule - the same one used for other drugs. Doctors didn’t know about the interaction. The result? A wave of preventable hospitalizations.Once the pharmacokinetic data came in - showing valproate cuts lamotrigine clearance by 50% - guidelines changed. The FDA added a black box warning. Prescribing manuals were rewritten. The number of serious rashes dropped by over 90%.
Today, the risk is low - but it’s not zero. And it’s still entirely dependent on how you start and adjust the dose. No genetic test, no blood screening, no fancy algorithm can replace the simple rule: slow down when valproate is involved.
Final Takeaway
Valproate and lamotrigine can be a great combo - for seizures, for mood, for quality of life. But they demand respect. Treat the dose like a precision instrument. Start low. Go slow. Watch for rashes. Stop immediately if one appears. The science is clear. The protocol is simple. The stakes are high.If you’re on both drugs, ask your doctor: “Are we following the valproate-adjusted lamotrigine titration schedule?” If they say yes - good. If they say no - ask why. Your skin, and possibly your life, depends on it.


Chad Kennedy
2 December / 2025I took lamotrigine with valproate for a year. Got a rash. Stopped both. Never went back. Simple.