Toxic Epidermal Necrolysis: Causes, Risks, and What You Need to Know
When your skin starts to peel off like a sunburn gone wrong, it’s not just a rash—it could be Toxic Epidermal Necrolysis, a rare, life-threatening skin condition where large areas of the epidermis detach from the body. Also known as Lyell's syndrome, it’s not something you can treat at home. This isn’t an allergic reaction you can shrug off with antihistamines. It’s a medical emergency that often starts with flu-like symptoms and quickly turns into a full-body skin crisis.
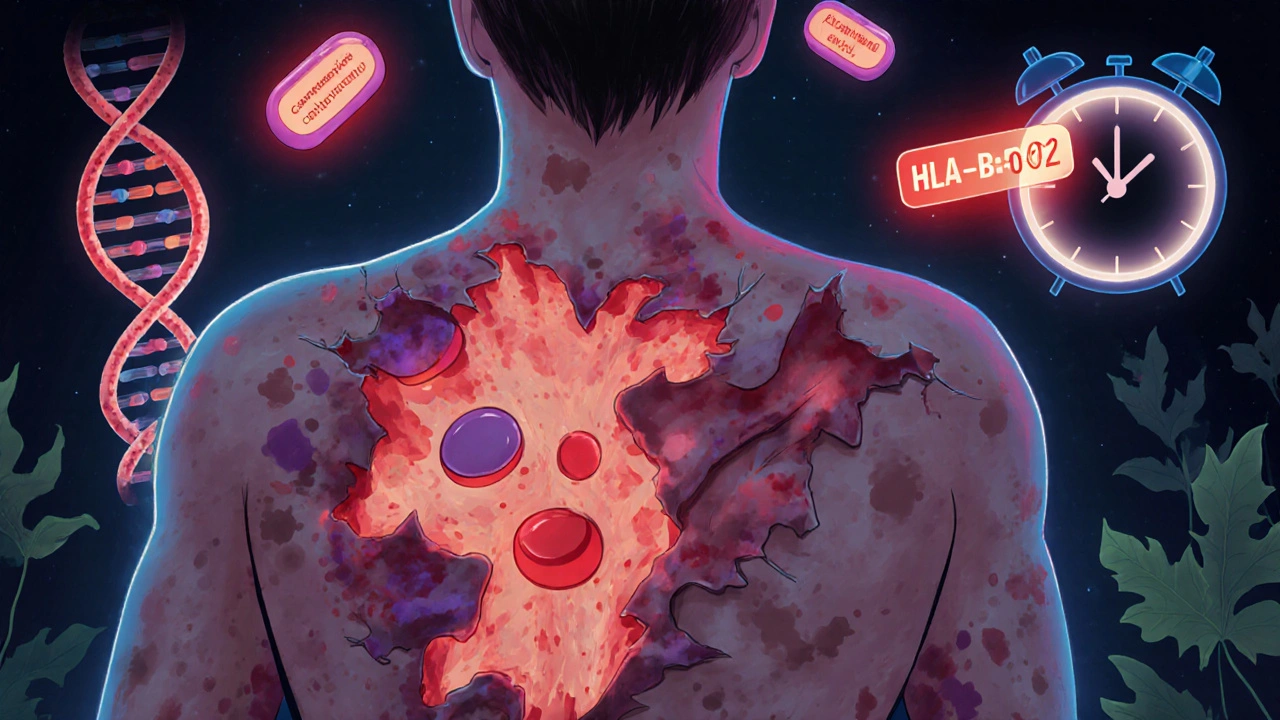
Most cases are triggered by medications, common drugs that are usually safe for most people but can cause catastrophic reactions in rare cases. Antibiotics like sulfonamides, anticonvulsants such as carbamazepine and lamotrigine, and pain relievers like allopurinol are the usual suspects. It’s not about taking too much—it’s about your body’s unique response. One pill, one dose, and suddenly your skin begins to fail. The risk is low, but the consequences are severe: over 30% of cases end in death without prompt hospital care.
People with certain genetic markers, like HLA-B*15:02, are at higher risk, especially those of Asian descent. But you can’t predict it before it happens. That’s why knowing the early signs matters—fever, burning eyes, sore throat, and a painful red rash that spreads fast. Within days, the top layer of skin blisters and sloughs off, leaving raw, exposed tissue. Think of it like a third-degree burn covering your whole body, but caused by a drug you took just days ago.
This is why reporting adverse drug events isn’t just paperwork—it’s saving lives. When someone reports a case of Toxic Epidermal Necrolysis to systems like FDA MedWatch, the official U.S. system for tracking dangerous side effects from drugs and medical products, it helps regulators spot patterns. One person’s tragedy can prevent another’s. That’s why posts on how to report side effects, like the one on MedWatch, aren’t just helpful—they’re critical.
There’s no cure, only aggressive treatment: stopping the drug immediately, ICU-level care, wound management, and sometimes IV immunoglobulins. Survival depends on speed. If you or someone you know starts peeling skin after starting a new medication, don’t wait. Don’t assume it’s just a rash. Go to the ER. Bring the medication bottle. Tell them everything you’ve taken in the last two weeks.
The posts here cover the broader landscape of drug safety—how medications interact, how to spot dangerous combinations, and how to report problems before they become disasters. You’ll find guides on serotonin syndrome from mixing supplements with SSRIs, on MAO inhibitor risks, and on how to switch antidepressants safely. These aren’t abstract warnings. They’re real stories hiding in plain sight. Toxic Epidermal Necrolysis is rare, but it’s not random. It’s the result of systems that work for most—but fail silently for a few. Understanding it isn’t just about one condition. It’s about learning how to protect yourself in a world full of medicines that promise help but can, in rare cases, turn deadly.
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis are rare but deadly drug reactions that cause skin and mucous membrane damage. Learn the warning signs, causes, treatments, and how genetic testing can prevent them.
View Details