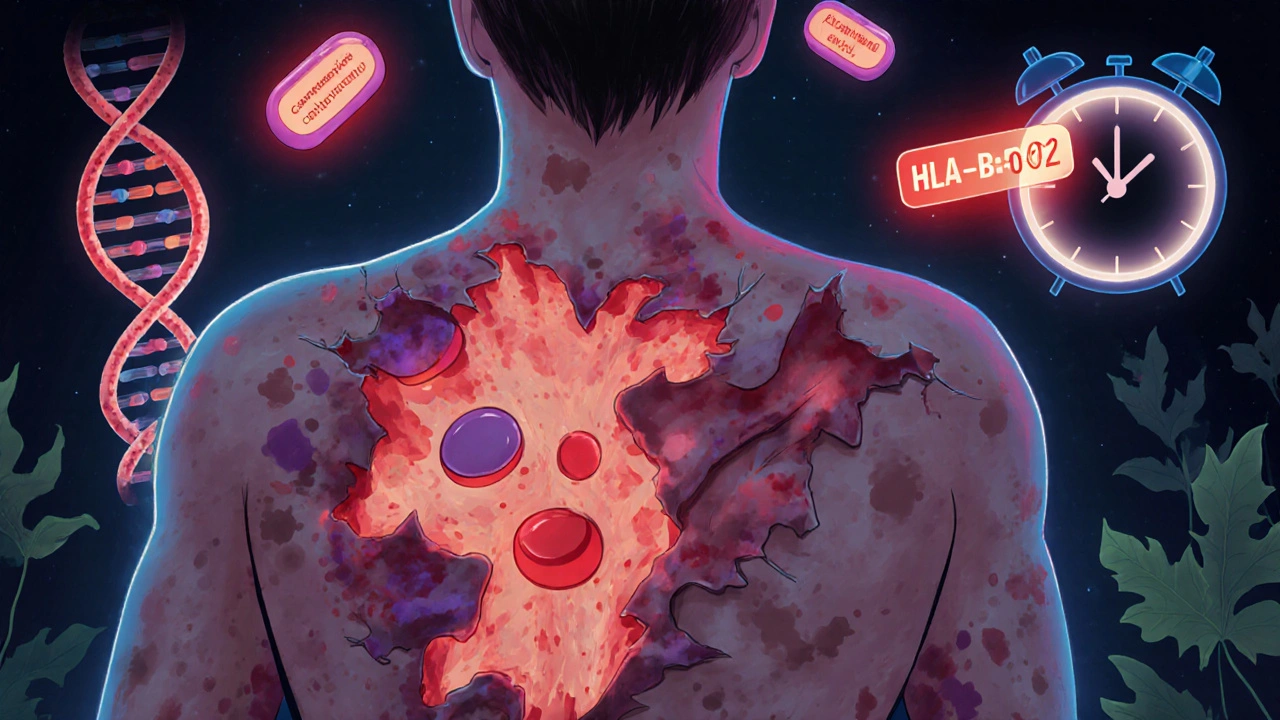
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis aren’t just rare skin conditions-they’re life-threatening emergencies triggered by your own body’s reaction to a medication. Think of it like your immune system going rogue, turning against your skin and mucous membranes. One moment you feel like you’ve got the flu; the next, your skin starts peeling off in sheets. It happens fast. It hurts terribly. And if you don’t recognize it early, it can kill you.
What’s the Difference Between SJS and TEN?
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are two ends of the same deadly spectrum. The only real difference is how much of your skin comes off. If less than 10% of your body surface area is affected, it’s SJS. Between 10% and 30%, it’s called SJS-TEN overlap. More than 30%? That’s TEN-the most severe form. In TEN, large areas of skin detach like a bad burn, leaving raw, open wounds that can get infected within hours.
Both start the same way: fever, sore throat, burning eyes, and a general feeling of being sick. It looks like the flu. But within 1 to 3 days, red or purple spots appear on your chest and back. These spots turn into blisters. Then the skin begins to slough off. The mucous membranes-your mouth, eyes, genitals-are almost always involved. You can’t swallow. Your eyes swell shut. Your urethra becomes inflamed. It’s not just a rash. It’s a full-body crisis.
What Causes It?
Over 80% of cases are caused by medications. The rest are linked to infections like Mycoplasma pneumoniae, especially in kids. But the big culprits? A few specific drugs keep showing up again and again.
- Carbamazepine (used for seizures and nerve pain)
- Allopurinol (for gout)
- Lamotrigine (another seizure and mood stabilizer)
- Trimethoprim-sulfamethoxazole (an antibiotic)
- NSAIDs like ibuprofen or naproxen (in rare cases)
Here’s the scary part: your genes can make you way more vulnerable. If you carry the HLA-B*15:02 gene variant, taking carbamazepine increases your risk of SJS/TEN by up to 1,000 times. That’s why in places like Taiwan and Thailand, doctors test for this gene before prescribing carbamazepine. The result? An 80% drop in cases. In the U.S., the FDA now recommends testing for HLA-B*58:01 before giving allopurinol to people of Asian descent. These tests are fast now-some labs can give results in four hours.
How Do Doctors Diagnose It?
There’s no single blood test for SJS/TEN. Diagnosis comes from three things: what you look like, what you’ve taken, and what the skin biopsy shows.
The biopsy is key. Under the microscope, you’ll see full-thickness death of the outer skin layer-keratinocyte necrosis-with almost no inflammation in the deeper layers. That’s different from staph infections or other blistering diseases. Doctors also check for the Nikolsky sign: if you gently rub the skin near a lesion and it peels off, that’s a red flag.
They’ll also use the SCORTEN score to predict survival. It looks at seven factors: your age, heart rate, how much skin is detached, blood sugar, kidney function, and more. If you have three or more risk factors, your chance of dying jumps to 35%. Five or more? It’s 90%. That’s why speed matters.

What Happens in the Hospital?
If you’re suspected of having SJS or TEN, you’re rushed to a burn unit or ICU. This isn’t a dermatology case-it’s a trauma case. Your skin is gone. You’re losing fluids like someone with third-degree burns. You’re at high risk for sepsis, pneumonia, and organ failure.
First step: stop every non-essential drug. Doctors go through your entire medication list, even things you’ve taken in the last month. They’ll often hold antibiotics, painkillers, supplements-everything. Then they start aggressive fluid replacement. You might need three to four times your normal daily fluid intake.
Wound care is delicate. No sticky bandages. No ointments that trap heat. Sterile, non-adherent dressings are used. Pain control is critical-you’re in extreme pain. Many patients need opioid infusions.
Ophthalmology is part of the team. Your eyes can scar permanently. Daily eye exams and lubricants are mandatory. Without them, you might lose vision. Up to 80% of survivors have long-term eye problems.
Treatment: What Works and What Doesn’t
There’s no magic bullet. For years, doctors used IVIG-high-dose antibodies-to try to shut down the immune attack. But large studies now show it doesn’t improve survival. Steroids? They might help early on, but they also raise your risk of deadly infections. So many hospitals avoid them.
Cyclosporine, a drug used in organ transplant patients, has shown promise. One 2016 study found it cut death rates from 33% to 12.5%. It works by calming down the immune cells that are killing your skin.
The most exciting new option? Etanercept. It blocks a protein called TNF-alpha that drives inflammation. A 2019 study treated 12 TEN patients with etanercept within 48 hours of symptoms starting. Zero died. In the past, that group would’ve had a 31% death rate. It’s not yet FDA-approved for this use, but it’s being used off-label in major centers.

What Happens After You Survive?
Surviving SJS or TEN doesn’t mean you’re back to normal. Far from it.
- 70% of survivors have lasting skin changes-patches that are darker or lighter than normal.
- 40% have scarring, especially on the neck, chest, and joints.
- 25% lose nails or grow them deformed.
- 15% develop urethral strictures-narrowing that makes peeing painful or impossible.
- 10% of women need surgery for vaginal adhesions.
- Up to 80% have chronic dry eyes, light sensitivity, or blurred vision.
- 40% develop PTSD from the trauma of being hospitalized, often for weeks, with no skin, in excruciating pain.
Recovery takes months. Some people need years of follow-up with dermatologists, ophthalmologists, urologists, and psychologists. Many can’t return to work. Some can’t even wear certain fabrics because their skin is so sensitive.
Can You Prevent It?
Yes-mostly by knowing your risk.
If you’re of Asian descent and your doctor wants to prescribe carbamazepine or allopurinol, ask about HLA testing. It’s a simple blood test. If you test positive for HLA-B*15:02, don’t take carbamazepine. There are safer alternatives. Same with HLA-B*58:01 and allopurinol.
Don’t ignore early warning signs. If you start a new medication and get a fever, sore throat, or eye irritation within the first two weeks, get checked. Don’t wait for the rash. Early recognition saves lives.
Keep a list of every drug you’ve ever taken, especially if you’ve had a bad reaction before. If you’ve had SJS/TEN once, you can’t take the same drug again. Ever. Cross-reactivity is common-even similar drugs can trigger another reaction.
Why This Matters
SJS and TEN are rare-only 1 to 6 cases per million people each year. But they’re not random. They’re preventable. They’re predictable. And they’re tied directly to how we prescribe drugs.
Doctors used to think these reactions were just bad luck. Now we know better. Genetics, timing, and medication choice all play a role. The tools to prevent them exist. The question is: are we using them?
For every person who survives, there are dozens more who never get diagnosed in time. And for every death, there’s a story of a missed warning sign, a delayed test, or a drug given without checking the patient’s genetic risk.
If you’re on long-term medication-especially for epilepsy, gout, or mental health-know your risks. Ask questions. Advocate for yourself. Because in this case, knowledge isn’t just power. It’s survival.
Can Stevens-Johnson Syndrome be caused by infections?
Yes, though it’s rare. About 10% of pediatric cases are triggered by infections, especially Mycoplasma pneumoniae. In adults, infections cause fewer than 20% of cases. Most cases-over 80%-are linked to medications. But if you’ve recently had a respiratory infection and develop a rash with fever and mouth sores, doctors will consider both possibilities.
How long does it take to recover from SJS or TEN?
The acute phase lasts 8 to 12 days, but full recovery takes months to years. Skin regrows in 2 to 4 weeks, but scarring, pigmentation changes, and organ damage can persist. Eye problems, dryness, and pain often last for life. Many survivors need ongoing care from multiple specialists. Returning to normal daily life can take 6 to 12 months, and some never fully regain their pre-illness quality of life.
Is SJS/TEN contagious?
No. It’s not an infection. You can’t catch it from someone else. It’s an immune reaction triggered by drugs or, rarely, infections in your own body. Even if you’re caring for someone with SJS/TEN, you’re not at risk of getting it yourself-unless you’re taking the same medication that caused it.
Can you get SJS/TEN from over-the-counter painkillers?
Yes, but it’s uncommon. NSAIDs like ibuprofen, naproxen, and celecoxib have been linked to cases, especially in people with a genetic predisposition. While the risk is far lower than with drugs like carbamazepine or allopurinol, it’s still possible. If you develop a rash, fever, or mouth sores after starting any new OTC medication, stop it and seek medical help immediately.
If I had SJS once, can I take similar drugs in the future?
Absolutely not. Once you’ve had SJS or TEN, you must avoid the drug that caused it-and often entire classes of similar drugs. For example, if carbamazepine triggered your reaction, you should avoid oxcarbazepine, phenytoin, and lamotrigine too. Cross-reactivity is common. Always tell every doctor you see about your history. Wear a medical alert bracelet if possible.
Are children at risk for SJS/TEN?
Yes, but less often than adults. Children make up about 10-15% of cases. In kids, infections like Mycoplasma pneumoniae are a more common trigger than drugs. However, when drugs are the cause, the same high-risk medications apply-especially antiepileptics and antibiotics. Pediatric cases are often misdiagnosed as viral rashes, leading to delays. If a child develops a fever and rash after starting a new medication, don’t wait-get them evaluated right away.


shubham seth
17 November / 2025Yo, this isn't just medical info-it's a goddamn wake-up call wrapped in a pharmacological landmine. I’ve seen guys on allopurinol for gout get shipped to burn units like they’re collateral damage in Big Pharma’s chess game. And no one’s talking about the fact that HLA testing costs less than a month’s supply of ibuprofen but hospitals still skip it like it’s a conspiracy. Wake up, America-your skin isn’t a suggestion, it’s your fucking organ.