Generic Substitution: What It Is and How It Saves You Money on Medications
When your doctor writes a prescription, you might get a generic substitution, the practice of replacing a brand-name drug with a chemically identical generic version. Also known as generic drug interchange, it’s one of the most straightforward ways to cut your prescription costs without losing effectiveness. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They’re not cheaper because they’re weaker—they’re cheaper because their makers didn’t pay for the original research, marketing, or patents.
Generic substitution isn’t just a trick to save money—it’s built into how the system works. The Hatch-Waxman Act, a 1984 law that created the modern pathway for generic drug approval gave companies a way to enter the market after patents expire, as long as they prove their version works the same. When multiple generic manufacturers enter the race, prices drop fast—sometimes by over 70%. That’s why a 30-day supply of metformin might cost $4 instead of $300. But not all substitutions are automatic. Some states let pharmacists swap generics without asking you, while others require your doctor’s permission. And if you’re on a drug like lamotrigine, an antiepileptic that can cause serious rashes if dosed wrong, your doctor might insist you stick with the same brand or generic to avoid tiny differences in fillers that could affect absorption.
Generic substitution doesn’t mean lower quality. It means smarter spending. But it also means paying attention. If you switch from one generic to another and notice side effects, it’s not just in your head—some generics use different inactive ingredients that can cause reactions in sensitive people. That’s why knowing how to spot a dispensing error, when the wrong pill is given out, even if it’s still a generic matters. It’s why carrying your meds in original containers during travel isn’t just a suggestion—it’s a safety rule. And it’s why understanding the difference between a side effect, a common, expected reaction and a true drug allergy, a dangerous immune response can keep you out of the ER.
What you’ll find below is a collection of real, practical guides that show how generic substitution touches every part of your medication experience—from how it drives down prices when multiple makers compete, to how it affects your liver if you’re on opioids, to why your pharmacist might ask if you want the generic version of your antidepressant. These aren’t theory pieces. They’re the kind of info you need when you’re holding a prescription, staring at the price tag, and wondering if you’re getting the same medicine—or just a cheaper copy.
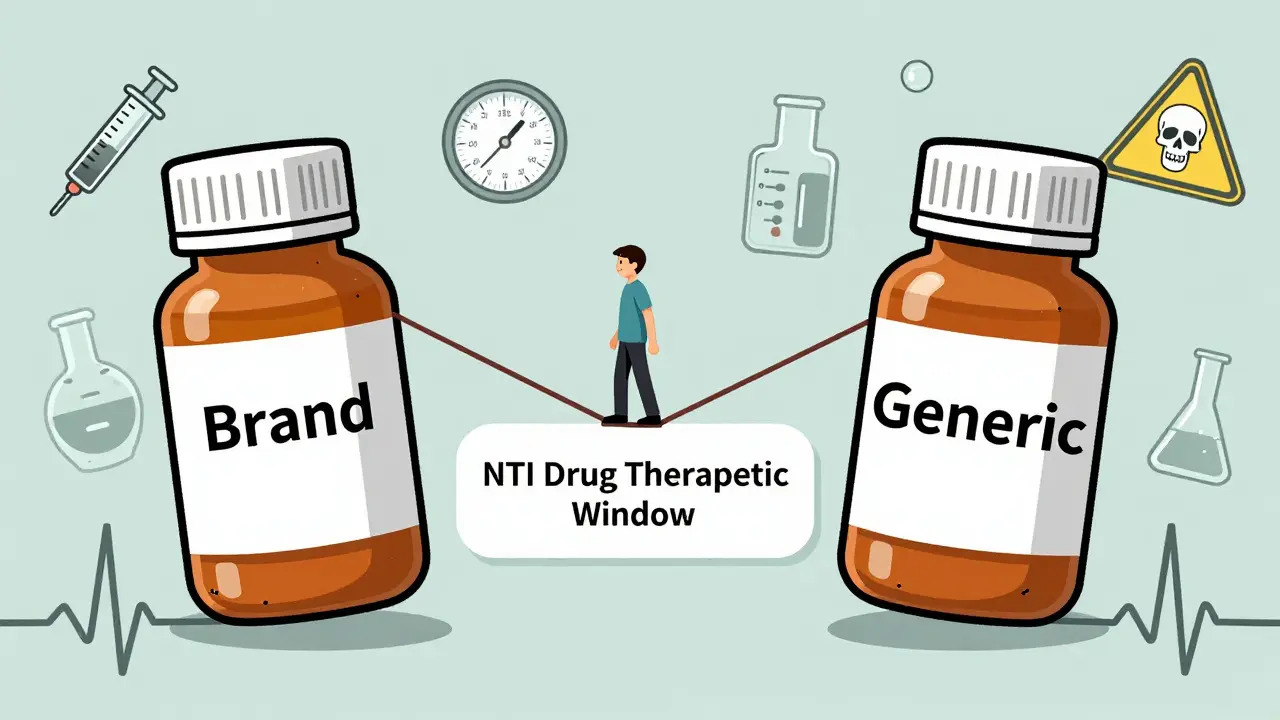
Studies show that switching to generic versions of narrow therapeutic index (NTI) drugs like warfarin, phenytoin, and cyclosporine can lead to dangerous fluctuations in blood levels. While some patients remain stable, others face seizures, organ rejection, or bleeding. Monitoring is critical after any switch.
View DetailsTrack how your body reacts when switching to generic medications with a simple medication journal. Learn what to record, why it matters, and how to use it to protect your health.
View Details