One glass of grapefruit juice in the morning might seem like a healthy start - but if you're taking certain medications, it could be dangerous. This isn't just a myth or a vague warning. Grapefruit juice can change how your body handles powerful drugs, sometimes raising their levels so high they cause serious harm - or even death. And it doesn’t take much: just 200 milliliters, about a cup, is enough to trigger a reaction. You don’t need to drink it daily. One serving, even hours before your pill, can be enough.
How Grapefruit Juice Changes How Your Body Processes Medications
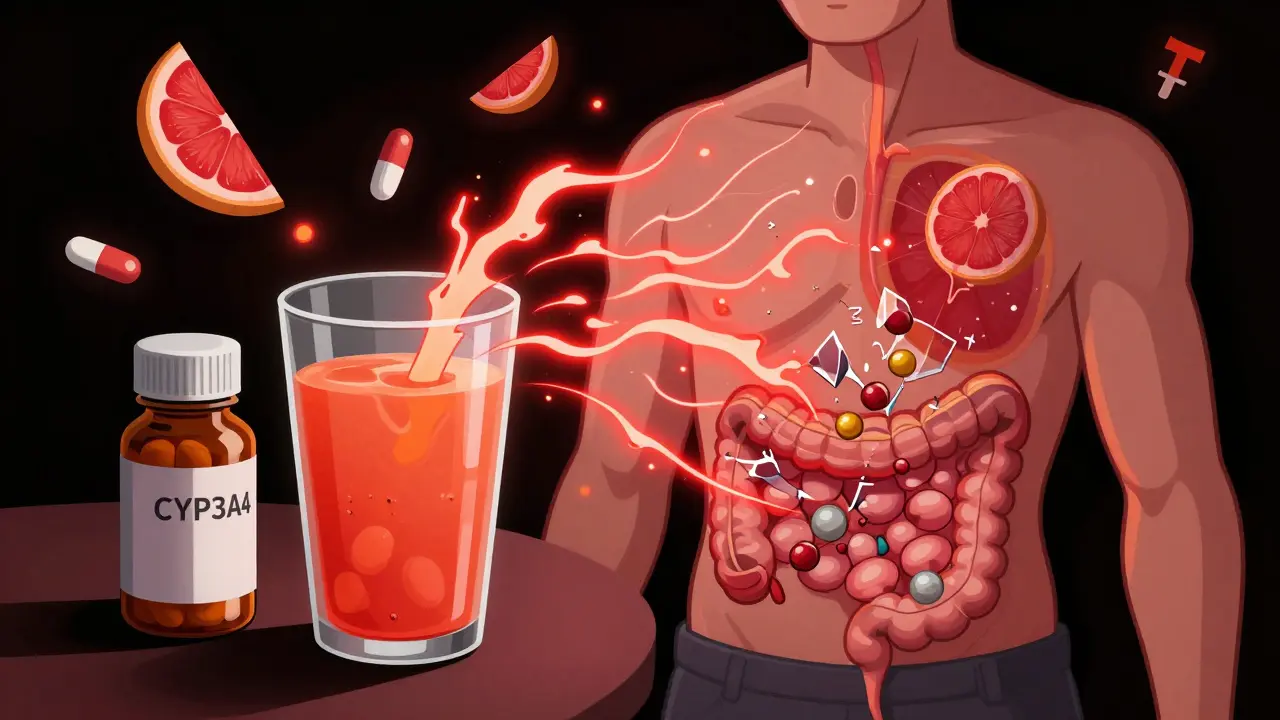
It all comes down to enzymes in your gut - specifically, CYP3A4. This enzyme normally breaks down many drugs before they enter your bloodstream, acting like a gatekeeper. Grapefruit juice doesn’t just slow this process; it shuts it down - permanently - for that day. The culprits are chemicals called furanocoumarins, mainly bergamottin and 6',7'-dihydroxybergamottin. These compounds bind to CYP3A4 and destroy it. Your body can’t fix the damage right away. It takes about three days for your gut to grow new enzymes.
What does that mean for you? If you’re taking a drug that CYP3A4 usually breaks down, that drug doesn’t get filtered out. Instead, it floods into your blood. A single glass of grapefruit juice can make simvastatin - a common cholesterol drug - reach 330% higher levels in your bloodstream. For felodipine, a blood pressure medication, levels can jump by 800%. That’s not a small bump. That’s the difference between a safe dose and a toxic one.
Which Medications Are Most at Risk?
Not all drugs are affected. But if your medication is processed by CYP3A4, you need to pay attention. The FDA has flagged 21 high-risk medications, and more than 85 are known to interact in some way. Here are the big ones:
- Statins: Simvastatin and lovastatin are dangerous with grapefruit. Atorvastatin has a moderate risk. But pravastatin, rosuvastatin, and fluvastatin? Safe. They use different pathways.
- Calcium channel blockers: Felodipine and nifedipine can cause dangerously low blood pressure or heart rhythm issues. Amlodipine? No major interaction.
- Immunosuppressants: Cyclosporine and tacrolimus - used after transplants - can lead to kidney damage if levels spike.
- Benzodiazepines: Oral midazolam can cause extreme sedation or breathing problems.
- Antiarrhythmics: Amiodarone can cause irregular heartbeats that turn deadly.
- Some antidepressants and antipsychotics: Sertraline, quetiapine, and others can build up to toxic levels.
Here’s the catch: you won’t always know. Labels don’t always warn you. In 2021, only 19% of prescription labels in the U.S. mentioned grapefruit - up from 12% in 2015, but still far from complete. Your pharmacist might not bring it up unless you ask.
It’s Not Just Juice - It’s the Whole Fruit and More
People often think they’re safe if they eat the fruit instead of drinking juice. Wrong. The same furanocoumarins are in the pulp and peel. Even a single grapefruit can trigger the reaction. Frozen concentrate? Same risk. Freshly squeezed? Same. There’s no safe form.
And it’s not just grapefruit. Seville oranges - the kind used in marmalade - contain the same chemicals. Pomelos? Also risky. But regular oranges, tangerines, and clementines? Safe. They don’t have furanocoumarins. If you’re unsure, stick to those.

Why Some People Are More at Risk Than Others
Not everyone reacts the same way. In one study, some people saw their felodipine levels jump 8-fold after grapefruit juice. Others? Barely a change. Why? Because people have different levels of CYP3A4 in their gut to begin with. The more you naturally have, the bigger the spike when it’s knocked out.
Genetics play a role too. A variant called CYP3A4*22 makes people more sensitive. Age matters. Older adults often take multiple medications and have slower enzyme repair. That’s why the American Geriatrics Society lists grapefruit interactions as a major concern for people over 65. In fact, 42% of adults over 65 take five or more drugs - and many of them are affected.
And here’s the sad part: even after being warned, 47% of patients keep eating grapefruit. Among seniors, that number jumps to 63%. They think, “I’ve been drinking it for years.” Or they forget. Or they don’t realize how long the effect lasts.
How Long Does the Effect Last?
This is where most people get it wrong. You can’t just wait an hour or two. The enzyme damage is irreversible. Your gut doesn’t heal overnight. It takes about 72 hours - three full days - for new enzymes to grow back.
So if you take a medication like simvastatin at night, and you drink grapefruit juice at breakfast, you’re still at risk. The juice you had 12 hours earlier is still blocking your enzymes. That’s why experts say: avoid grapefruit entirely during treatment. Not “space it out.” Not “have it on the weekends.” Avoid it completely.
There’s one exception: OATP transporter interactions. For drugs like fexofenadine (Allegra), grapefruit juice blocks absorption, making the drug less effective. For those, a 4-hour gap helps. But for the vast majority of drugs - the dangerous ones - timing doesn’t help. Only avoidance does.

What Should You Do?
Step one: Check your meds. Look up your prescriptions on the FDA’s list or ask your pharmacist. Don’t assume you know. Many people don’t realize their cholesterol pill, blood pressure med, or anti-anxiety drug is on the list.
Step two: If you’re on a high-risk medication, stop grapefruit entirely. No exceptions. Swap it for oranges, apples, or berries. There are plenty of healthy alternatives.
Step three: Tell your doctor and pharmacist. If you’ve been drinking grapefruit juice for years, let them know. They may be able to switch you to a safer drug. For example, switching from simvastatin to rosuvastatin removes the risk entirely. Many patients have made this switch safely through programs like the American Pharmacists Association’s ‘Grapefruit-Free Alternatives’ initiative.
Step four: Educate your family. Especially if you’re caring for an older relative. They might not understand the risk. A 2021 study found only 28% of patients could name even one medication affected by grapefruit - even after being told.
The Bigger Picture: Why This Isn’t Going Away
This isn’t just a personal health issue. It’s a public health blind spot. In the European Union, grapefruit interactions cause about 85 serious adverse events each year - and 12 deaths between 2000 and 2019. Globally, they make up 1.3% of all reported drug reactions.
Pharmacies now use software that flags grapefruit interactions. Electronic health records pop up alerts. Drug manufacturers are reformulating pills to reduce risk. Some are even working on gene-edited grapefruit that don’t contain furanocoumarins - still in trials, but promising.
But none of that matters if patients don’t know. And too many still don’t. The science is clear. The warnings exist. The alternatives are safe and available. What’s missing is consistent, clear communication - and the discipline to change a habit that seems harmless.
It’s easy to ignore a warning on a label. But this isn’t about being careful. It’s about survival. One glass of juice. One pill. One day of carelessness. And the consequences can be irreversible.
Can I drink grapefruit juice if I take my medication at night and juice in the morning?
No. Grapefruit juice destroys enzymes in your gut that last for about 72 hours. Even if you take your pill at night and juice in the morning, the enzyme damage from the juice is still active. The interaction isn’t about timing - it’s about total avoidance. If your medication is on the high-risk list, skip grapefruit completely.
Are all citrus fruits dangerous with medications?
No. Only grapefruit, Seville oranges (used in marmalade), and pomelos contain furanocoumarins. Regular oranges, tangerines, clementines, and lemons are safe. Don’t assume all citrus is the same. If you’re unsure, stick to sweet oranges or apples.
Does it matter if I eat the fruit instead of drinking the juice?
No. The harmful chemicals are in the pulp, peel, and juice. Eating a whole grapefruit has the same effect as drinking a glass of juice. There’s no safe way to consume it if you’re on a high-risk medication.
Can I just cut back instead of quitting completely?
No. Even small amounts - as little as 200 mL - can trigger a dangerous interaction. The effect isn’t dose-dependent in a linear way. One glass can cause an 800% spike in some drugs. Cutting back doesn’t reduce risk enough. Complete avoidance is the only safe option.
What if I’ve been drinking grapefruit juice for years and feel fine?
That doesn’t mean you’re safe. Some people have naturally low levels of CYP3A4 enzymes, so the interaction doesn’t affect them much. But you can’t know your risk without testing. A sudden change - like adding another medication, aging, or liver changes - can turn a harmless habit into a life-threatening one. Don’t rely on past experience. Check with your doctor.
Are there safer alternatives to my medication if I want to keep drinking grapefruit juice?
Yes. For many high-risk drugs, there are safe alternatives. For example, switch from simvastatin to rosuvastatin or pravastatin. Swap felodipine for amlodipine. Replace cyclosporine with tacrolimus (if appropriate). Talk to your doctor - many patients have successfully switched without losing effectiveness. The American Pharmacists Association has helped over 14,000 people make this change.
What to Do Next
If you’re on medication, don’t wait for a warning label. Take five minutes today. Look up your prescriptions on the FDA’s list of drugs affected by grapefruit. Or ask your pharmacist - they’re trained to spot this. If you’re taking more than one medication, the risk multiplies. Elderly patients, especially, need to be proactive.
There’s no magic pill or clever trick. The science is settled. The risk is real. And the solution is simple: skip grapefruit. Your body will thank you.

Darren McGuff
8 January / 2026Just had a patient come in last week who didn’t know grapefruit juice could wreck his statin. He’d been drinking it for 15 years. Turned out his CK levels were through the roof. Pharmacist flagged it - he was shocked. This isn’t just a warning. It’s a silent killer. Always ask your pharmacist. They’re the unsung heroes of drug safety.