Have you ever taken a pill with breakfast, only to feel like it didn’t work? Or skipped a dose because you weren’t sure whether to take it before or after eating? You’re not alone. Many people don’t realize that what’s on your plate can make or break how well your medicine works.
Why Food Changes How Medicines Work
Your stomach and intestines don’t just digest food-they also control how drugs enter your bloodstream. When you eat, your body shifts into digestion mode. Blood flow changes. Stomach acid levels drop. Gastric emptying slows down. All of this affects how fast and how much of your medicine gets absorbed. For some drugs, food helps. For others, it blocks them. A high-fat meal can delay absorption by up to two hours. Calcium in dairy can bind to antibiotics and stop them from working. Fiber can trap pills and carry them out before they’re absorbed. Even the pH of your stomach changes after eating, which matters for drugs that need acid to dissolve. The FDA requires drug makers to test every new medication with a standardized high-fat meal (about 800-1,000 calories, half from fat) to see how food affects it. If absorption changes by more than 20%, the label must say whether to take it with or without food. About 35% of new drugs approved between 2015 and 2022 came with these kinds of instructions.When to Take Medicine on an Empty Stomach
Some medications simply don’t work well with food. These usually need to be taken at least one hour before or two hours after eating. Levothyroxine, used for thyroid problems, is one of the most common. Food can reduce its absorption by 30-55%. That means even if you take the right dose, your thyroid levels might stay low. That’s why doctors tell you to take it first thing in the morning with a full glass of water-no coffee, no toast, no cereal. Wait at least 30 minutes before eating. Tetracycline antibiotics like doxycycline are another example. Calcium in milk, yogurt, cheese, and even some orange juices binds to these drugs and prevents them from being absorbed. One Reddit user reported a recurring UTI that only cleared up after they stopped taking doxycycline with their morning yogurt. The fix? Wait two hours after eating dairy before taking the pill. Itraconazole, an antifungal, needs stomach acid to work. High-fat meals raise stomach pH, making it less acidic. That cuts absorption by 40%. This drug works best on an empty stomach, ideally in the morning before breakfast. Levothyroxine and tetracycline are the big ones, but others like atenolol, alendronate (for osteoporosis), and ciprofloxacin also need empty stomachs. Always check your label or ask your pharmacist.When Food Helps Your Medicine Work Better
Not all drugs hate food. Some actually need it. Griseofulvin, an older antifungal, absorbs 200-300% better with a high-fat meal. That’s because it’s fat-soluble-fat helps dissolve it so your body can absorb it. Without food, it just passes through. Nitrofurantoin, used for urinary tract infections, absorbs 40% better when taken with food. It also causes less nausea and stomach upset when taken with a snack. Cefpodoxime, another antibiotic, sees a 50-60% boost in absorption with meals. Same goes for ritonavir and other HIV drugs-food helps them reach effective levels in your blood. Sulfonylureas like glipizide are diabetes pills that trigger insulin release. If you take them on an empty stomach, your blood sugar can crash. That’s why you must take them 30 minutes before eating. Skipping meals after taking them puts you at risk for dangerous hypoglycemia-below 70 mg/dL-which happened to 23% of users in one study. NSAIDs like ibuprofen and naproxen are another case. They can irritate your stomach lining. Taking them with food reduces the risk of ulcers and acid reflux by more than 70%. One patient survey found stomach pain dropped from 42% to 12% when taken with meals.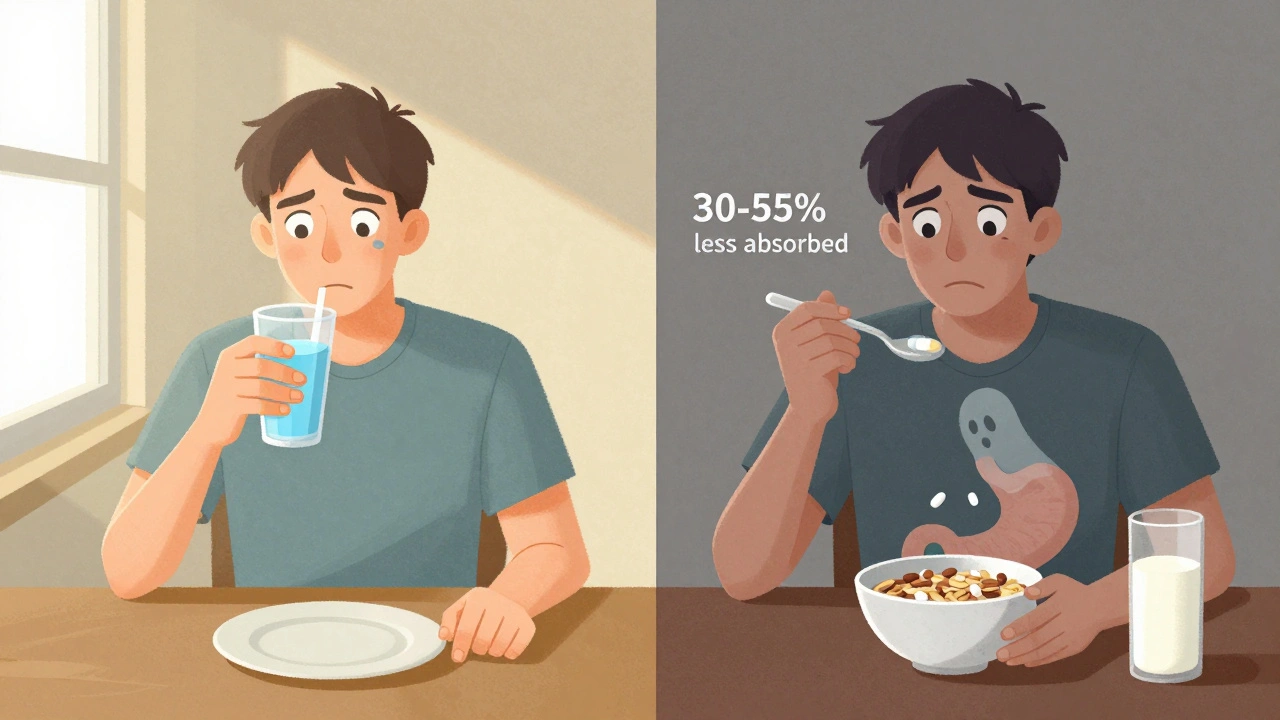
What Does “With Food” Really Mean?
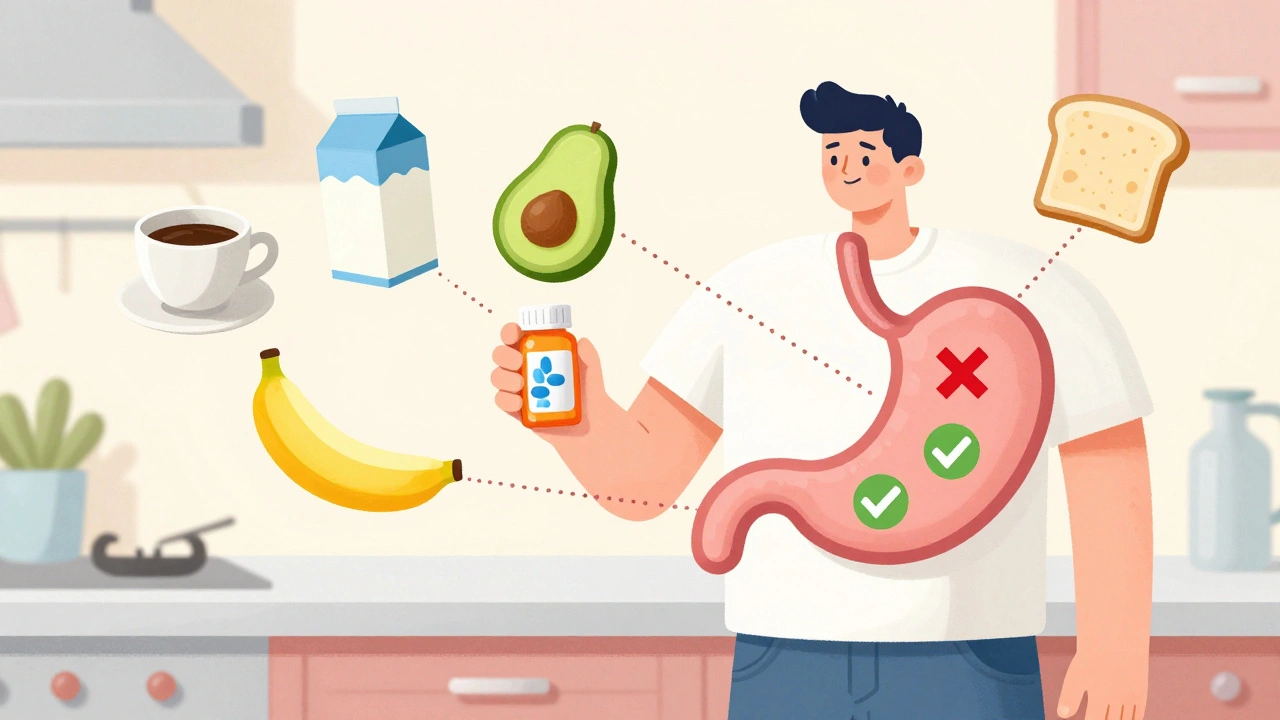
Here’s where people get confused. “Take with food” doesn’t always mean a full meal. For some drugs, like atazanavir (an HIV medication), a small snack of 200-300 calories is enough. That could be a banana, a handful of nuts, or a slice of toast. You don’t need a steak dinner. But for others, like griseofulvin, you need real fat-avocado, eggs, cheese, or a burger. A piece of fruit won’t cut it. The Australian Prescriber defines “with food” as taking the medicine within 30 minutes of starting your meal. That gives your body time to start digesting and release bile and enzymes that help absorption. The problem? A 2023 Express Scripts report found 45% of patients misunderstand this. One man took his HIV meds with a cup of black coffee-thinking that counted as “food.” His drug levels were too low. He ended up with a resistant strain.Timing Mistakes That Hurt Your Health
People make the same mistakes over and over.- Taking levothyroxine with coffee or calcium-fortified orange juice.
- Swallowing doxycycline with yogurt or milk.
- Skipping glipizide because they’re not hungry.
- Waiting two hours after breakfast to take a drug that needs to be taken with food.
How to Get It Right Every Time
Here’s how to avoid common traps:- Read the label. Look for “take on empty stomach,” “take with food,” or “take 30 minutes before meals.”
- Ask your pharmacist. They’re trained to catch these details. Don’t assume your doctor told you everything.
- Set phone alarms. If you take levothyroxine in the morning, set a reminder for 60 minutes before breakfast. For meds taken with food, set a reminder 15 minutes before your meal.
- Keep a log. Write down what you ate and when you took your pills. You might spot patterns-like why your blood pressure spiked after a fatty lunch.
- Be consistent. If you take a drug with food, always take it with food. If you take it empty, always do it empty. Inconsistency causes fluctuating drug levels.
What’s Changing in 2025
Guidelines are getting smarter. The FDA now includes plant-based and gluten-free meals in food-effect testing. That’s because more people eat these diets. A high-fat vegan meal might affect a drug differently than a cheeseburger. Digital tools are catching up, too. Apps like Medisafe and MyTherapy now have food-timing reminders. Users who turn them on see 27% fewer timing errors. New tech is coming. Ingestible sensors that track stomach pH and emptying speed are being tested. One 2023 trial showed 38% better absorption consistency for pH-sensitive drugs when timing was adjusted in real time. And now, researchers are looking at chronopharmacology-timing meds not just with meals, but with your body’s natural rhythms. Some blood pressure pills work better at night. Some cancer drugs are more effective in the morning. Future labels might say: “Take 30 minutes before breakfast, between 7-8 a.m.”Who’s at Highest Risk?
Older adults taking five or more medications are most vulnerable. One study found they have a 65% higher chance of food-drug interactions. Why? They juggle pills for blood pressure, diabetes, cholesterol, arthritis, and more. Some need food. Others need no food. Some need water only. It’s a minefield. If you or someone you care for is on multiple meds, ask for a medication review. A pharmacist can map out which pills go with meals, which go without, and which need spacing.Bottom Line
Food isn’t just fuel. It’s part of your medicine routine. Taking a pill the wrong way-whether with milk, coffee, or on an empty stomach-can mean it doesn’t work. Or worse, it harms you. The fix isn’t complicated. Know your meds. Read the label. Ask your pharmacist. Set a reminder. Be consistent. Your body absorbs drugs based on what’s happening inside you. Don’t leave it to chance.Can I take my medication with coffee?
It depends on the drug. Coffee can interfere with thyroid meds like levothyroxine and some antibiotics. For most drugs, wait at least 30 minutes after taking the pill before drinking coffee. If your label says “take on an empty stomach,” coffee counts as something to avoid until after your dose.
What if I forget to take my pill at the right time?
If you missed taking a drug that needs an empty stomach and just ate, wait at least two hours before taking it. If you took a food-dependent drug without eating, have a small snack (like a banana or crackers) and take it then. Never double up unless your doctor says so. When in doubt, call your pharmacist.
Do all antibiotics need to be taken on an empty stomach?
No. Only certain ones do. Tetracyclines (like doxycycline) and fluoroquinolones (like ciprofloxacin) should be taken on an empty stomach. Others, like amoxicillin, azithromycin, and cefpodoxime, work better with food. Always check the label or ask your pharmacist.
Can I take my pill with juice?
Some juices interfere. Grapefruit juice can make some heart and cholesterol drugs too strong-sometimes dangerously so. Orange juice can block absorption of certain antibiotics and thyroid meds. Stick to water unless your doctor says otherwise.
Why do some pills need fat to work?
Some drugs are fat-soluble, meaning they dissolve better in fat than in water. Griseofulvin, itraconazole, and certain HIV meds need fat to be absorbed properly. Without it, your body might pass most of the dose out without using it. That’s why a full-fat meal is required-not just any snack.
Is it okay to take medicine with alcohol?
No. Alcohol can increase side effects like drowsiness, dizziness, and liver damage. It can also interfere with how your body breaks down certain drugs. Even if your label doesn’t say “avoid alcohol,” it’s safest to skip it when taking new medications.


Arun kumar
1 December / 2025so i took my levothyroxine with my chai one morning and thought my thyroid was acting up... turns out it was just the milk and cardamom messing with absorption. dumb move. now i drink coffee 45 mins after. small wins.
also why does no one talk about how hard it is to remember this when you’re half-asleep and your kid is screaming for cereal?