Pharmacy Business Models: How Generic Drugs, Discounts, and Competition Shape Your Rx Costs
When you pick up a prescription, you’re not just getting medicine—you’re interacting with a complex pharmacy business models, the systems and strategies pharmacies and manufacturers use to sell, distribute, and profit from medications. Also known as pharmaceutical distribution models, these structures determine everything from how much you pay at the counter to whether a drug even reaches your shelf. It’s not magic. It’s math, competition, and regulation—and it’s changing fast.
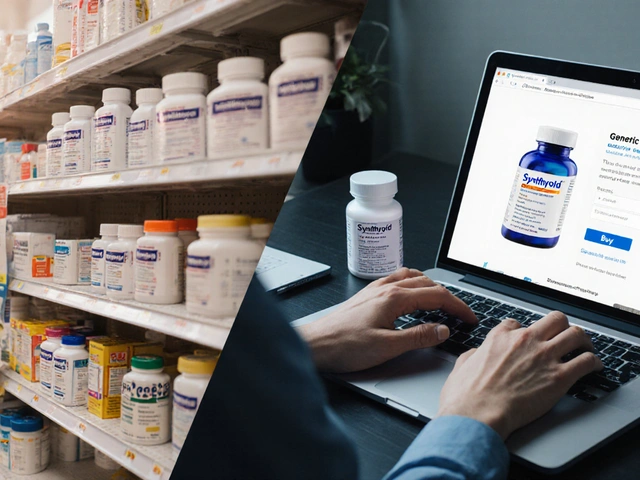
At the heart of this system is generic drug competition, when multiple companies make the same drug after the brand-name patent expires. When four or more makers enter the market, prices often drop over 70%. That’s not theory—it’s real data from the FDA and independent studies. But when only one or two companies make a generic, prices stay high. That’s why some pills cost $5 and others $50, even if they’re chemically identical. This isn’t just about big pharma—it’s about who controls supply and how fast new players can get into the game. Then there’s prescription discounts, like GoodRx and pharmacy coupons, which let you pay less out-of-pocket by bypassing insurance networks. These tools work great for generics but often don’t help with brand-name drugs. They’re not scams—they’re workarounds built because the system is broken. And they’re everywhere because patients are fed up with surprise bills. Behind the scenes, pharmacy safety, the practices that prevent dispensing errors and protect patients. One study found patient counseling catches 83% of mistakes before they leave the counter. That’s not just good service—it’s a business necessity. A single error can cost a pharmacy millions in lawsuits and reputation damage. So the best-run pharmacies don’t just fill scripts—they verify them, explain them, and train staff to spot look-alike drugs.
These three forces—competition, discounts, and safety—are the pillars of modern pharmacy. They’re why you can buy amoxicillin for $4, why you get a coupon for your statin, and why your pharmacist asks if you’ve ever had a reaction to penicillin. They’re also why some drugs disappear from shelves when no one wants to make them cheaply, and why your insurance won’t cover a drug your doctor swears by. The system isn’t perfect, but understanding how it works lets you make smarter choices. You don’t need to be an expert. You just need to know where the leverage points are.
Below, you’ll find real stories from people who’ve navigated this system—how they saved money on prescriptions, avoided dangerous drug interactions, reported harmful side effects, and fought back when things went wrong. These aren’t abstract theories. They’re lived experiences from patients, pharmacists, and caregivers who’ve seen how pharmacy business models play out on the ground. Whether you’re paying out-of-pocket, fighting insurance denials, or just trying to understand why your meds cost what they do, this collection gives you the tools to take control.
Direct-to-consumer generic pharmacies are cutting out middlemen to offer lower prices, faster delivery, and simpler refills for everyday medications. Here’s how they work, who’s using them, and why they’re changing U.S. healthcare.
View Details