MAO inhibitors (MAOIs) are one of the oldest classes of antidepressants, but they’re also among the most dangerous if used carelessly. These drugs work by blocking the enzyme that breaks down key brain chemicals like serotonin, norepinephrine, and dopamine. That’s how they help with depression - but that same mechanism can turn everyday medications, supplements, and even foods into silent killers.
Why MAOIs Are Different
Most antidepressants today - like SSRIs (fluoxetine, sertraline) - tweak how the brain reabsorbs serotonin. MAOIs do something more drastic: they shut down the enzyme that destroys serotonin and other neurotransmitters entirely. That means more of these chemicals stay active in your brain, which can lift mood. But it also means your body loses its natural safety valve. If something else pushes serotonin or norepinephrine levels even higher - say, a cold medicine or a cheese sandwich - your system can go into overdrive.This isn’t theoretical. In the 1950s, when MAOIs first hit the market, patients died from sudden, massive spikes in blood pressure after eating aged cheese. That’s not a myth. It’s documented in hospital records. Today, the same risks persist, even though MAOIs are rarely prescribed anymore. Less than 1% of antidepressant prescriptions in the U.S. are for MAOIs, and most of those go to patients who’ve tried everything else without success.
The Two Deadly Risks: Hypertensive Crisis and Serotonin Syndrome
There are two life-threatening reactions you must avoid with MAOIs. The first is a hypertensive crisis. This happens when tyramine - a compound found in aged, fermented, or spoiled foods - builds up in your blood. Normally, your body breaks down tyramine using the same enzyme MAOIs block. When that enzyme is shut down, tyramine triggers a flood of norepinephrine. Blood pressure can shoot up 50 to 100 points in under two hours. Systolic pressure can hit 200-250 mmHg. That’s enough to cause a stroke, heart attack, or brain hemorrhage.The second risk is serotonin syndrome. This occurs when too much serotonin accumulates in your nervous system. It can start with mild symptoms like shivering, diarrhea, or restlessness - but it can escalate quickly to high fever (over 106°F), muscle rigidity, seizures, and organ failure. Death rates for severe cases range from 2% to 12%. And it doesn’t take much to trigger it.
Medications That Can Kill You When Mixed With MAOIs
Here are the most common and dangerous drugs that should never be taken with MAOIs:- SSRIs and SNRIs - Fluoxetine (Prozac), sertraline (Zoloft), venlafaxine (Effexor). Combining these with MAOIs can cause serotonin syndrome within hours. You must wait at least 14 days after stopping an MAOI before starting an SSRI. For fluoxetine, wait five weeks - its effects linger much longer.
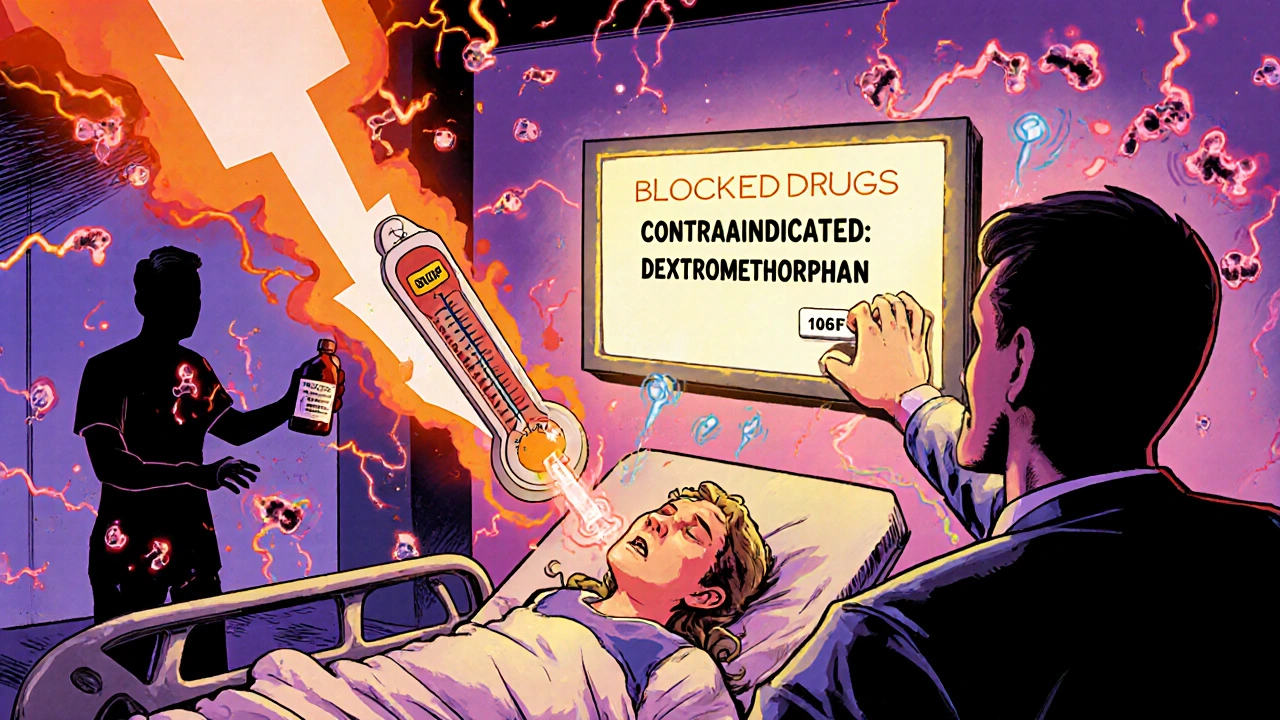
- Dextromethorphan - Found in over 100 cough syrups and cold pills. A single 30mg dose in someone on phenelzine has triggered severe agitation, high fever, and hospitalization. The FDA issued a warning in 1992, but many people still don’t know.
- Tramadol, meperidine, methadone - These painkillers are absolute no-gos. A 32-year-old man on selegiline needed intubation after taking 50mg of tramadol. He survived, but not everyone does.
- Linezolid - This antibiotic, used for stubborn infections, also inhibits monoamine oxidase. Taking it with an MAOI can cause serotonin syndrome. It’s been linked to fatal cases since at least 2008.
- Phenylephrine and pseudoephedrine - Found in decongestants like Sudafed and many “sinus” or “cold” formulas. These directly raise blood pressure. With an MAOI, that effect becomes dangerous.
- Ephedra and ephedrine - Even though the FDA banned ephedra in 2004, some supplements still contain it. A single dose has sent people to the ICU with blood pressure over 220/120.
Supplements and Herbal Products to Avoid
Many people think “natural” means safe. That’s not true with MAOIs.- St. John’s Wort - Used for mild depression, but it boosts serotonin. Combined with MAOIs, it’s a recipe for serotonin syndrome.
- 5-HTP - A supplement that turns into serotonin in your body. One patient on phenelzine took 200mg of 5-HTP and developed a fever of 40.5°C, blood pressure of 220/110, and ended up in the ICU.
- SAMe - Sold as a mood booster. Also increases serotonin. Not safe with MAOIs.
- Ginseng - Documented since 1985 to cause mania and tremors in people on MAOIs. Some cases may have been worsened by caffeine contamination, but the risk is real.
Food Risks: It’s Not Just Cheese
You’ve probably heard to avoid aged cheese. But that’s only the tip of the iceberg.- Aged cheeses - Cheddar, blue cheese, parmesan, gouda (especially over 6 months old). One ounce can contain 15mg of tyramine - enough to trigger a crisis.
- Fermented soy - Soy sauce, miso, tempeh. One tablespoon of soy sauce has 1-30mg tyramine.
- Cured meats - Pepperoni, salami, sausage. Up to 100mg tyramine per ounce.
- Draft and tap beer - Contains 8-20mg tyramine per 12oz. Bottled beer is usually safer.
- Red wine - Chianti and other aged wines have about 8mg per 5oz glass.
- Overripe fruits - Bananas, avocados, figs. The riper they are, the more tyramine they develop.
There’s a threshold: 10-25mg of tyramine can trigger a reaction. That’s not much. One slice of aged cheddar or a splash of soy sauce could be enough. But here’s a critical exception: the selegiline patch (Emsam) at the lowest dose (6mg/24hr) doesn’t require dietary restrictions. Studies show patients can eat normally without risk at this level. Higher doses still require caution.
What Doctors Are Doing to Prevent Accidents
Because of past deaths, systems have been built to stop these mistakes before they happen.- Electronic health records now have hard stops - if you’re on an MAOI, your doctor can’t prescribe tramadol or dextromethorphan. The system blocks it.
- The FDA requires black box warnings on all MAOI labels - the strongest warning they issue.
- Many psychiatrists give patients wallet cards listing all contraindicated drugs. A 2020 survey showed 78% of psychiatrists do this.
- Switching from an MAOI to another antidepressant requires a 14-day washout. For fluoxetine, it’s five weeks because the drug sticks around in your system for so long.
But the system isn’t perfect. A 2021 study found that 34% of primary care doctors didn’t know dextromethorphan was dangerous with MAOIs. That’s a huge gap. Many patients see their primary care provider for a cold - not their psychiatrist. And if the doctor doesn’t know, the patient might get a dangerous prescription.
Who Still Gets MAOIs Today?
MAOIs aren’t first-line anymore. They’re reserved for treatment-resistant depression, atypical depression (with oversleeping, overeating, mood reactivity), or severe anxiety disorders when other drugs have failed. About 92% of MAOI prescriptions come from psychiatrists. Only 8% come from general doctors.The selegiline patch (Emsam) now makes up 68% of all MAOI prescriptions. Why? Because it’s safer. The skin absorbs the drug slowly, and at the lowest dose, it doesn’t interfere with tyramine metabolism. That’s a game-changer.
There’s also moclobemide - a reversible MAOI used in Europe and Canada. It’s much safer with fewer food and drug interactions. But it was never approved in the U.S. because clinical trials showed only modest benefits compared to SSRIs.
What You Should Do If You’re on an MAOI
If you’re taking an MAOI - or thinking about it - here’s what you need to do:- Get a full list of all medications and supplements you take - including over-the-counter, herbal, and vitamins.
- Give that list to your psychiatrist. Don’t assume they know what you’re taking.
- Ask: “Is this safe with my MAOI?” - even if it’s something you’ve used for years.
- Carry a wallet card listing contraindicated drugs. Many pharmacies will print one for free.
- Wear a medical alert bracelet that says “MAOI - avoid tyramine, SSRIs, dextromethorphan, linezolid.”
- If you feel sudden headache, chest pain, stiff muscles, or high fever - go to the ER immediately. Don’t wait.
MAOIs aren’t evil drugs. For some people, they’re the only thing that works. But they demand respect. A single mistake - a cold medicine, a cheese plate, a supplement - can be fatal. Knowledge isn’t optional. It’s survival.
Can I take Tylenol with an MAOI?
Yes, acetaminophen (Tylenol) is generally safe with MAOIs. It doesn’t affect serotonin or norepinephrine levels. Avoid NSAIDs like ibuprofen or naproxen if you have high blood pressure or are on other medications that affect clotting, but Tylenol itself carries no known interaction risk with MAOIs.
Is caffeine dangerous with MAOIs?
Caffeine isn’t directly dangerous with MAOIs, but it can worsen side effects like jitteriness, rapid heartbeat, or high blood pressure. If you’re already at risk for hypertensive crisis, too much coffee or energy drinks could push you over the edge. Limit intake to 1-2 cups per day.
Can I drink alcohol while on an MAOI?
Avoid alcohol. It can cause a sudden spike in blood pressure when combined with MAOIs. Red wine, in particular, contains tyramine. Even beer - especially draft or tap - can trigger a reaction. If you must drink, stick to small amounts of clear spirits like vodka or gin, and avoid any fermented or aged drinks.
What if I accidentally take a contraindicated drug?
Call your doctor or go to the ER immediately. Don’t wait for symptoms. If you took dextromethorphan, tramadol, or a decongestant, symptoms can appear within 30 minutes. Early signs include headache, rapid heartbeat, sweating, or restlessness. Emergency treatment may include benzodiazepines, cooling measures, or blood pressure-lowering drugs.
Are there any MAOIs that are safer than others?
Yes. The selegiline patch (Emsam) at the 6mg/24hr dose has minimal dietary restrictions and lower interaction risk. Oral MAOIs like phenelzine and tranylcypromine are much more dangerous. Reversible MAOIs like moclobemide (not available in the U.S.) are safer still, but they’re not approved here.
Can I stop an MAOI cold turkey?
No. Stopping abruptly can cause withdrawal symptoms like anxiety, irritability, dizziness, or even rebound depression. Always taper under your doctor’s supervision. If you’re switching to another antidepressant, follow the 14-day (or 5-week for fluoxetine) washout period exactly.
Do MAOIs interact with birth control or hormones?
There’s no direct interaction between MAOIs and birth control pills, patches, or IUDs. However, hormonal changes can affect mood, which may influence how well the MAOI works. Always tell your doctor if you start or stop hormonal therapy.



henry mariono
17 November / 2025I’ve been on selegiline for 3 years now. The patch is a game-changer. I eat blue cheese, drink tap beer, and even had a slice of salami last week. No issues. Just make sure you’re on the 6mg dose - higher and you’re back to the old rules. Doctors need to stress this more.