Every year, thousands of people end up in the hospital not because their meds don’t work, but because they took them at the wrong time. You might be taking a pill for your thyroid, another for your bones, and a third for your stomach-all perfectly normal. But if you swallow them all together at breakfast, you could be blocking absorption, reducing effectiveness, or even causing harm. The solution isn’t always to stop one drug. Often, it’s as simple as timing them right.
Why Timing Matters More Than You Think
Not all drug interactions are created equal. Some happen because two drugs clash chemically in your bloodstream-like warfarin and metronidazole, where one slows down how fast the other breaks down. Those can’t be fixed by waiting a few hours. But about 20-30% of interactions are different. They’re called time-dependent drug interactions (TDDIs). These happen because one drug gets in the way of another being absorbed in your gut. For example, if you take ciprofloxacin (an antibiotic) with an antacid like Tums, the calcium and magnesium in the antacid bind to the antibiotic before it can be absorbed. Studies show this can cut the antibiotic’s effectiveness by up to 90%. But if you wait just two hours between them, absorption goes back to normal. No dose change. No drug swap. Just timing. The same goes for levothyroxine, the common thyroid medication. If you take it with iron, calcium, or even coffee, your body absorbs less than half of what it should. Research in the Journal of Clinical Endocrinology & Metabolism found that spacing levothyroxine at least four hours away from these substances keeps absorption above 95%. That’s the difference between feeling tired all day and having energy.Common Medications That Need Space
Here are the most frequent offenders-and how to separate them:- Antibiotics (tetracycline, ciprofloxacin, levofloxacin): Don’t take within 2-3 hours of dairy, antacids, iron, or zinc supplements. These minerals lock onto the antibiotic like glue.
- Levothyroxine (Synthroid, Tirosint): Take on an empty stomach, at least 4 hours before or after calcium, iron, multivitamins, or soy products. Even coffee can interfere-wait 30-60 minutes after taking it.
- Bisphosphonates (alendronate, risedronate): These osteoporosis drugs need to be taken with a full glass of water, first thing in the morning, and you must wait 30 minutes before eating, drinking, or taking anything else. Otherwise, they won’t reach your bones.
- Cholesterol drugs (ezetimibe, statins): Some statins work better when taken at night, but if you’re also on bile acid sequestrants like cholestyramine, space them at least 4 hours apart. The sequestrant can trap the statin before it’s absorbed.
- Antifungals (itraconazole, ketoconazole): These need stomach acid to work. Don’t take them with antacids, H2 blockers (like famotidine), or proton pump inhibitors (like omeprazole) unless you separate them by at least 2 hours.
What Timing Won’t Fix
Timing helps with absorption problems. It doesn’t help with metabolism problems. If your liver breaks down one drug too slowly because another drug blocks the enzyme (like warfarin and amiodarone, or simvastatin and grapefruit juice), waiting hours won’t change anything. Those interactions are about chemistry in your bloodstream, not your stomach. In those cases, your doctor might need to adjust the dose, switch you to a different drug, or monitor you more closely with blood tests. For example, if you’re on warfarin and need to take metronidazole for a bacterial infection, your INR levels could spike dangerously. You can’t just space them out-you need a blood test and possibly a lower warfarin dose.Real-World Success Stories
At UCSF Medical Center, pharmacist Jane Chen noticed a pattern: elderly patients on iron supplements kept developing anemia-even though they were taking the pills. Turns out, they were swallowing them with their proton pump inhibitor (PPI) for heartburn. The PPI raised stomach pH, making iron harder to absorb. She set up a simple protocol: iron in the morning on an empty stomach, PPI after lunch. Within 18 months, iron deficiency cases dropped by 32%. Another win came from a hospital in Minnesota. Nurses noticed patients on multiple daily meds were skipping doses because the schedule was too confusing. They started using color-coded pill organizers with separate compartments for morning, afternoon, and evening-and built in time buffers between interacting drugs. Timing errors dropped by 43%.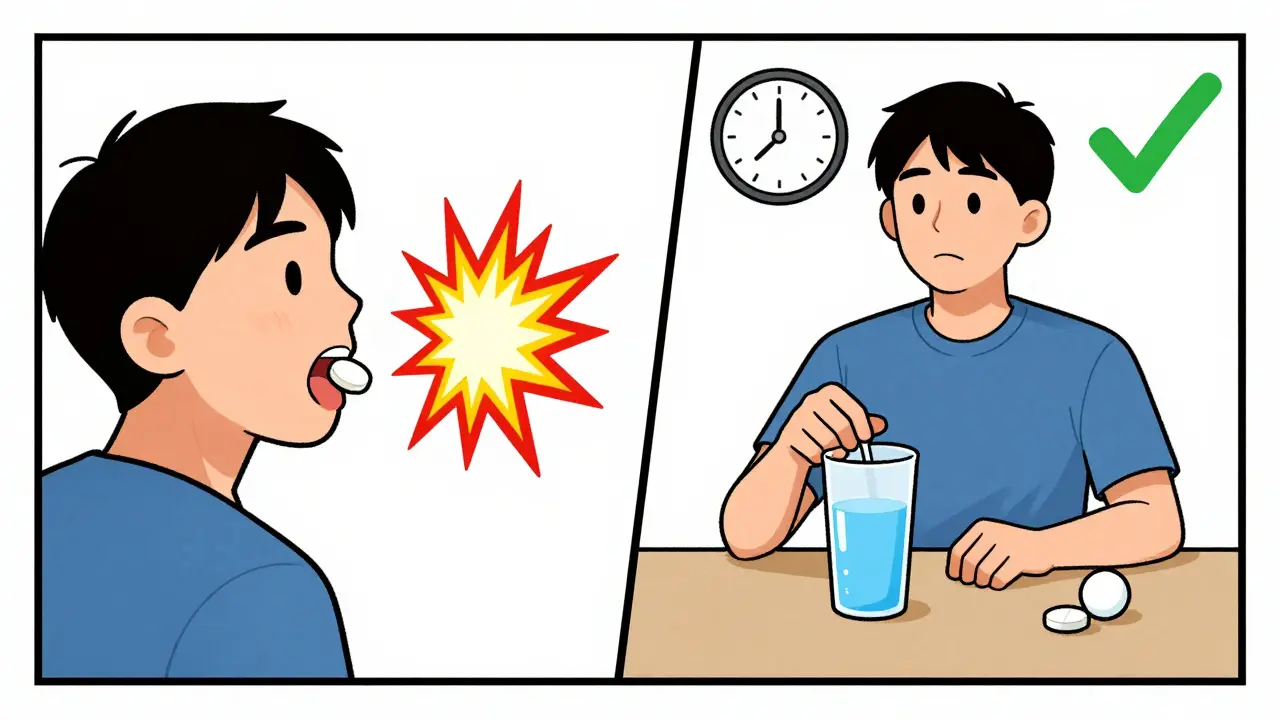
Why Patients Struggle-and How to Fix It
The biggest problem isn’t the science. It’s the complexity. People on five or more medications often have to juggle different timing rules. One pill must be taken before breakfast. Another must wait two hours after. A third can’t be taken with milk. A fourth needs to be taken at bedtime. It’s easy to forget, mix up, or feel overwhelmed. A 2022 survey on AllNurses.com found that 40% of patients didn’t follow their timing instructions. Why? 68% of those over 65 said they forgot which meds needed spacing. Others said their doctors never explained it clearly. Some didn’t even know timing mattered. The fix? Simple tools. Digital apps like Medisafe or MyTherapy let you set custom alerts for each medication, with notes like “Wait 2 hours before calcium.” One 2021 trial with 1,245 patients showed adherence to timing rules jumped 57% when using these apps. Pill organizers with multiple compartments also help. Instead of one big box, use a 7-day organizer with AM/PM slots-or even a four-compartment daily box. Label each section with the time and purpose: “Thyroid-AM, empty stomach,” “Iron-10 AM,” “Antibiotic-2 PM, no dairy.”What Your Doctor or Pharmacist Should Do
You shouldn’t have to figure this out alone. Every time you get a new prescription, ask: “Does this interact with any of my other meds? Do I need to take it at a different time?” Doctors and pharmacists now have access to tools like Lexicomp or Micromedex that flag time-dependent interactions. Hospitals in the U.S. use computerized systems that alert providers if a new drug clashes with an existing one based on timing. But community pharmacies? Only 37% have these alerts built in. If you’re on multiple meds, ask for a full medication review. Bring a list of everything you take-including supplements, OTC painkillers, and herbal products. A pharmacist can map out a daily schedule that avoids clashes. Many insurance plans now cover this service.Getting Started: A 3-Step Plan
1. List every medication-prescription, over-the-counter, vitamins, herbs. Include dosage and how often you take it. 2. Check for timing conflicts. Use a trusted source like the FDA’s drug interaction database or Lexicomp. Look for interactions marked as “absorption-based” or “time-dependent.” 3. Create a simple schedule. Use a whiteboard, phone app, or printed chart. Group meds by time of day. Add notes: “Wait 2 hours,” “Take on empty stomach,” “Avoid dairy.” Start with your top 3 most important meds. Get those timing rules right first. Then add the rest. Don’t try to fix everything at once.
The Bigger Picture
The U.S. spends over $1 billion a year treating preventable drug interactions. The National Academy of Medicine estimates that if everyone followed proper timing rules, we could prevent 115,000 to 178,000 adverse events by 2028. That’s not just savings-it’s lives. It’s not about being perfect. It’s about being aware. You don’t need to memorize every interaction. You just need to know: Some meds need space. Ask when you’re unsure.Frequently Asked Questions
Can I take my blood pressure pill with my thyroid pill in the morning?
It depends. Most blood pressure meds (like lisinopril or amlodipine) don’t interfere with levothyroxine. But if you’re taking a beta-blocker with calcium or iron supplements, space them out. Always check with your pharmacist. The safest approach is to take levothyroxine alone on an empty stomach, then wait 30-60 minutes before anything else-including other pills.
What if I forget and take my antibiotic with dairy?
Don’t panic. One mistake won’t ruin your treatment. But don’t just take another dose right away. Wait until your next scheduled time. If you’re on a short course (like 7 days), finish the full prescription as directed. If you’re on a longer course or have symptoms that aren’t improving, call your doctor. They might want to check if the infection is responding.
Do herbal supplements cause timing problems too?
Yes. St. John’s wort can reduce the effectiveness of many drugs, including antidepressants and birth control pills. Calcium supplements from bone health formulas can block antibiotics. Even magnesium in some sleep aids can interfere with thyroid meds. Always list supplements on your medication list-even if you think they’re “natural.”
Is it okay to take all my pills at night to simplify things?
Only if none of them have timing restrictions. Levothyroxine, bisphosphonates, and some antibiotics must be taken in the morning on an empty stomach. Taking them at night defeats the purpose. If you’re trying to simplify, talk to your doctor about switching to once-daily alternatives that don’t conflict. But never change your schedule without professional advice.
How do I know if my medication has a timing warning?
Check the patient information leaflet inside the pill bottle. Look for phrases like “take on an empty stomach,” “avoid antacids,” or “separate from calcium by 2 hours.” Your pharmacist can also review the label with you. If you’re unsure, ask: “Is there a specific time I should take this to avoid problems with my other meds?”



Dusty Weeks
1 January / 2026bro i took my levothyroxine with my coffee this morning and now i feel like a zombie 🤯 why does no one tell you this stuff? i thought coffee was just for vibes