Twenty years ago, an HIV diagnosis meant a death sentence. Today, it’s a chronic condition-manageable, predictable, and far from the stigma it once carried. The shift didn’t happen overnight. It came from decades of research, failed trials, and breakthroughs that changed everything. Now, people living with HIV aren’t just surviving-they’re thriving. And the newest treatments are making life not just better, but simpler.
From Daily Pills to Twice-Yearly Injections
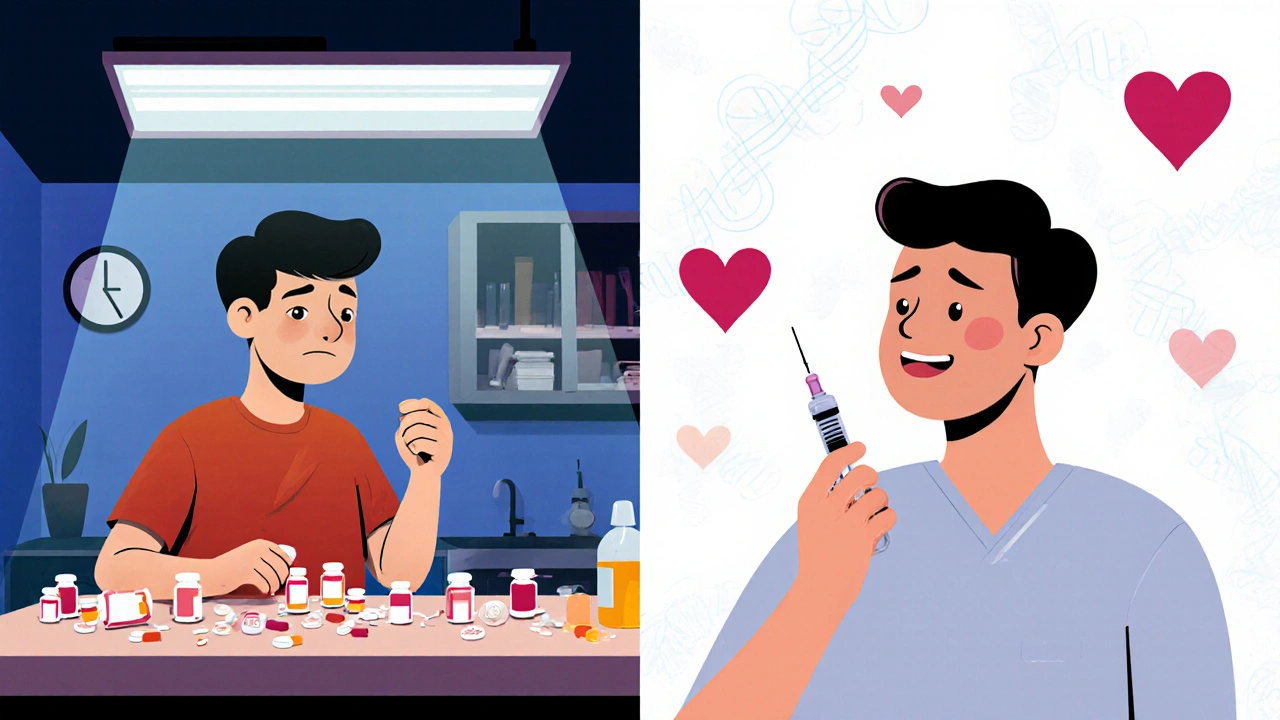
The standard for HIV treatment for over 25 years was taking one or more pills every single day. For many, it worked. But adherence was a constant struggle. Miss a dose, and the virus could bounce back. For others, the daily ritual became a mental burden-a reminder of a condition they didn’t ask for.
That changed with lenacapavir. Approved as Sunlenca for treatment in 2022 and as Yeztugo for prevention in June 2025, this drug is the first capsid inhibitor. It doesn’t just block the virus-it traps it. Lenacapavir interferes with the protein shell that protects HIV’s genetic material, stopping it from replicating. And here’s the game-changer: a single injection lasts six months.
Now, a new combo called LTZ-lenacapavir plus two broadly neutralizing antibodies (teropavimab and zinlirvimab)-is pushing boundaries even further. In trials presented at CROI 2025, it suppressed the virus in 98.7% of patients after 48 weeks. That’s better than daily pills. And instead of 12 clinic visits a year for monthly shots, you only need two. For someone juggling work, family, or mental health, that’s not just convenient-it’s life-changing.
The Leading Medications Today
While long-acting therapies are the future, most people still start with daily pills. Here’s what’s on the table:
- Biktarvy: A single tablet with bictegravir, emtricitabine, and tenofovir alafenamide. It’s small-just 459 mg-and doesn’t need boosting. That means fewer side effects and less strain on kidneys. Approved in 2018, it’s still the most prescribed regimen in the U.S.
- DELSTRIGO: Doravirine with lamivudine and tenofovir disoproxil fumarate. A good option for people with kidney issues, since it avoids the more nephrotoxic form of tenofovir.
- Sunlenca (lenacapavir): The first capsid inhibitor. Given as a subcutaneous injection every six months. Requires cold storage (-20°C), which has slowed rollout in clinics without proper facilities.
- Yeztugo: The same drug as Sunlenca, but approved for prevention. It’s PrEP with a twist-no daily pill, just two shots a year.
Other drugs are in the pipeline. Merck’s DOR/ISL (doravirine and islatravir) is a once-daily two-drug combo that’s showing promise for people with heart risks. ViiV Healthcare is testing VH-184 and VH-499, but neither matches lenacapavir’s twice-yearly dosing.
Quality of Life: More Than Just Viral Suppression
Suppression isn’t the only goal. It’s about peace of mind.
A 2025 survey from the Positive Peers app-used by over 150,000 people with HIV-found that 92% of those on long-acting treatments rated their satisfaction at 8 out of 10 or higher. Compare that to 76% on daily pills. Why? Because the psychological weight of daily medication lifted.
One Reddit user, u/HIVWarrior2020, wrote: “After 12 years of daily pills, the twice-yearly injection has eliminated my treatment-related anxiety completely.” That’s not just a quote. It’s a pattern. People report less shame, fewer panic checks for pill bottles, and more freedom to travel, date, or just live without the constant reminder.
There’s a cost, though. Injections can cause mild pain or swelling at the site. About 28% of users in the survey reported this-but 94% said it was worth it. Most reactions fade within 48 hours with ice and ibuprofen.
Access and Equity: The Big Hurdle
Here’s the uncomfortable truth: these breakthroughs are expensive. Biktarvy costs about $69,000 a year in the U.S. Yeztugo is $45,000. For context, the World Health Organization says generic versions could be produced for $25 per person per year.
That’s a thousand-fold difference.
In the U.S., 38% of patients have switched to long-acting options as of mid-2025. In Europe, it’s 12%. In sub-Saharan Africa-where 70% of all HIV cases live-it’s under 2%. Why? Cold chain storage. Clinic access. Cost. Training for health workers.
The WHO addressed this in July 2025, recommending that community health workers administer lenacapavir injections in low-resource areas. That’s a smart move. But implementation is slow. Only 43% of U.S. clinics could offer Sunlenca after the June 2025 rollout-up from 17%-because many didn’t have freezers or trained staff.
Dr. Mark Harrington of the Treatment Action Group put it bluntly: “Without urgent action on pricing, these breakthroughs will remain out of reach for the majority of people who need them.”
What’s Next? The Road to 2030
The data is clear: long-acting therapies are the future. By 2030, experts predict 75% of people with HIV in high-income countries will use them. In low-income countries, that number could hit 40%-if generic versions become widely available.
There’s even talk of a functional cure. ViiV’s IMPAACT 2009 trial in March 2025 showed three out of 25 participants maintained viral suppression after stopping all treatment. It’s not a cure yet, but it’s a sign we’re getting closer.
Meanwhile, Gilead’s LTZ regimen is on track for full FDA approval in early 2026. If it gets there, it won’t just be a treatment-it’ll be a prevention tool, a lifestyle changer, and a global health milestone.
Getting Started: What You Need to Know
If you’re considering switching from daily pills to a long-acting regimen:
- Ask your provider if you’re a candidate. You need to be virally suppressed for at least six months.
- Plan for a 4-week overlap. You’ll still take your pills while the injection builds up in your system.
- Check clinic availability. Not all places stock lenacapavir. Call ahead.
- Ask about support programs. Gilead offers patient assistance, and some insurers cover the full cost.
- Prepare for the injection. It’s quick, but you might feel sore for a day or two. Ice helps.
For prevention, Yeztugo is now an option for those at high risk-men who have sex with men, transgender individuals, sex workers, and partners of people living with HIV. No daily pill. Just two shots a year. That’s a game-changer for prevention.
Final Thoughts: Hope Is Here
HIV isn’t cured. But it’s no longer a sentence. The drugs today are more effective, less toxic, and far less intrusive than ever before. People aren’t just living longer-they’re living fuller lives.
The challenge now isn’t science. It’s access. It’s cost. It’s making sure the next generation doesn’t have to choose between their health and their dignity.
With the right policies, the right pricing, and the right commitment, we could end the HIV epidemic within a decade. The tools are here. The question is: will we use them?


swatantra kumar
19 November / 2025So now we got HIV treatment that needs a freezer and costs more than my car? 😅 Guess I’ll just keep my daily pills and my dignity. At least I don’t need a lab to take my medicine. 🤷♂️