Statins for Elderly: What You Need to Know About Safety, Benefits, and Alternatives
When doctors prescribe statins for elderly, a class of cholesterol-lowering drugs used to reduce cardiovascular risk. Also known as HMG-CoA reductase inhibitors, they’re among the most common medications given to older adults to prevent heart attacks and strokes. But for seniors, the line between benefit and risk isn’t always clear. Many people over 70 take statins without ever asking if they truly need them—or what the hidden downsides might be.
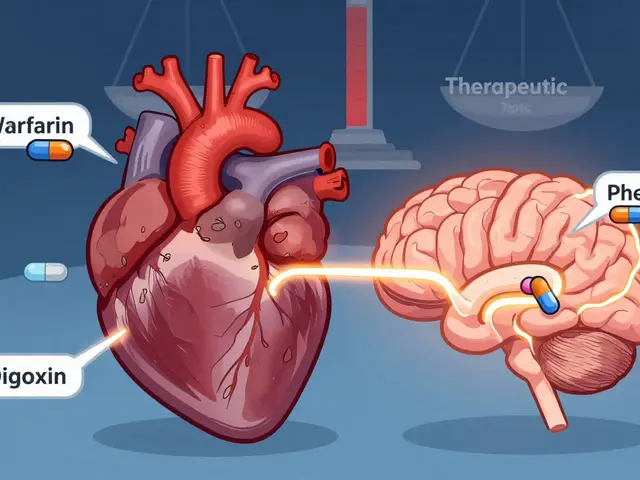
Not all elderly patients respond the same way. statin side effects, common issues like muscle pain, fatigue, and memory fog. Also known as myopathy, these reactions become more likely with age, especially when combined with other medications. A 78-year-old woman on a statin for high cholesterol might also be taking blood pressure pills, a blood thinner, or a pain reliever. Each of those can interact with statins, raising the chance of liver stress or muscle damage. And unlike younger people, seniors often don’t report mild muscle aches until they can’t climb stairs or get out of a chair.
elderly heart health, the focus on preventing cardiovascular events in older adults through medication and lifestyle. Also known as cardiovascular risk management in seniors, it’s not just about lowering numbers—it’s about quality of life. Studies show that for people over 75 with no history of heart disease, statins may not extend life or prevent heart attacks any better than a healthy diet and regular walking. That doesn’t mean statins are useless for seniors—it means they’re not a one-size-fits-all fix. If you’ve had a heart attack, stroke, or blocked artery, statins are still a powerful tool. But if your only issue is a cholesterol number that’s a bit high, the risks might outweigh the benefits.
Many older adults take statins because their doctor said so, not because they understand why. And when side effects hit, they often blame aging instead of the pill. Muscle weakness? "Just getting older." Brain fog? "That’s normal at my age." But these aren’t always normal. Sometimes, stopping the statin for a few weeks brings back energy, strength, and clarity. That’s not aging—it’s a drug reaction.
There are alternatives. For some seniors, switching to a lower-dose statin, adding ezetimibe, or focusing on diet and movement works just as well—without the side effects. Omega-3s, soluble fiber, and daily walking can lower LDL cholesterol without a prescription. And if you’re already on a statin, you can talk to your doctor about checking your CK levels, testing for vitamin D deficiency, or trying a different type of statin that’s gentler on muscles.
This collection of articles doesn’t just list facts—it gives you real, practical insights. You’ll find guides on how to recognize dangerous drug interactions, what to do if you feel worse after starting a statin, and how to talk to your doctor about tapering or switching. You’ll see how multiple generic manufacturers keep these drugs affordable, and why some seniors benefit far more than others. You’ll learn what the data really says about statins for people over 80, and how to weigh the risks without being scared or misled.
Statins for elderly patients can save lives—but only when they’re used wisely. This isn’t about saying "no" to medication. It’s about asking the right questions so you or your loved one doesn’t trade one problem for another.
Pravastatin is one of the safest statins for older adults, with fewer muscle side effects and drug interactions than alternatives. Learn how it compares, who benefits most, and what to watch for.
View Details