Sclerosis: What to Watch For and How to Manage It
Sclerosis simply means hardening or scarring in body tissue. You’ve probably heard it most with multiple sclerosis (MS) or systemic sclerosis (scleroderma). Both can change how you feel day to day, but they act differently and need different care. This page helps you spot common signs, know what tests to expect, and get practical tips for living better.
Quick symptom checklist
Symptoms vary by type, but here are common warning signs to mention to your doctor: numbness or tingling, unexplained muscle weakness, balance or vision problems, long-lasting fatigue, joint stiffness, tight or shiny skin patches, and trouble swallowing or breathing. If you get new or worsening symptoms over days to weeks, call your care team. Small changes can matter.
Doctors usually start with a physical and neurological exam, blood tests to rule out other causes, and imaging like MRI for MS or CT for internal issues. Sometimes nerve tests (EMG) or a skin/lab biopsy are used. Getting a clear diagnosis cuts down trial-and-error and speeds up the right treatment.
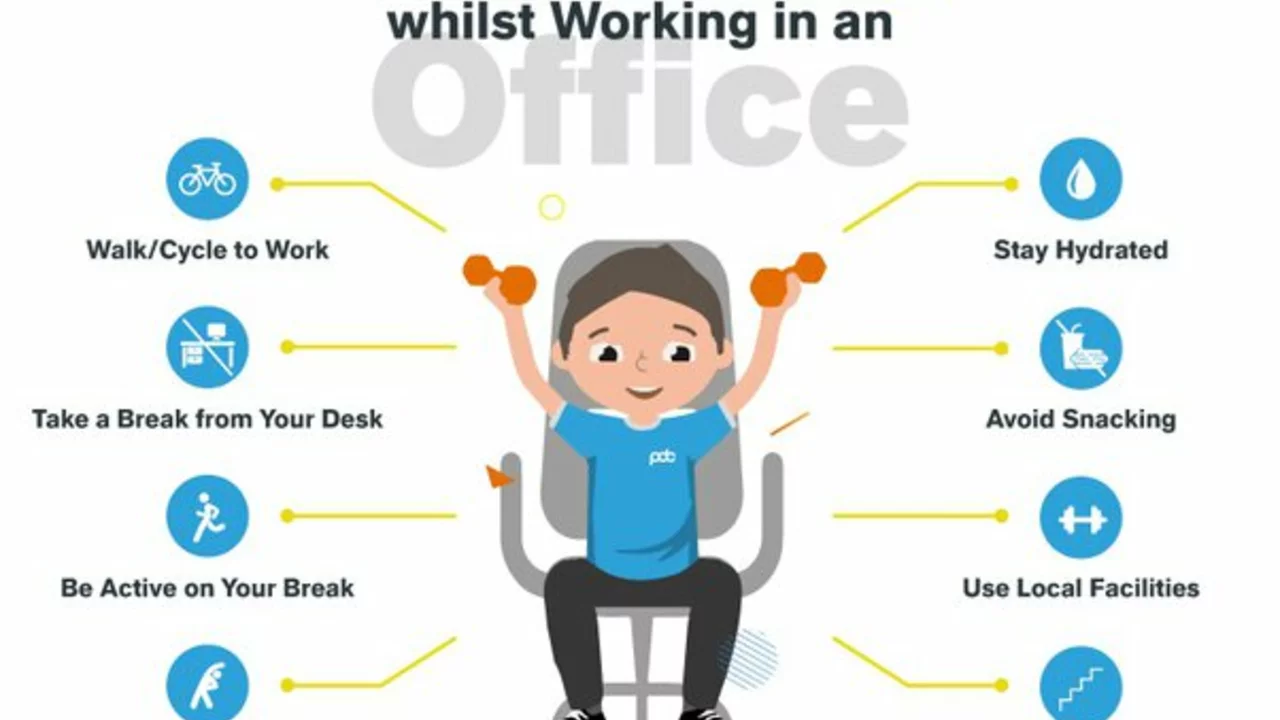
Practical steps for day-to-day management
Treatment usually mixes disease-specific drugs, symptom control, and rehab. Disease-modifying drugs aim to slow progression in some sclerosis types; steroids or short courses of other meds treat flares. For symptoms—pain, muscle spasms, bladder or bowel issues—there are reliable options your specialist can tailor to you. Keep a simple symptom diary: note what triggers flare-ups, how long symptoms last, and which meds help. That makes clinic visits far more productive.
Fatigue is one of the most common complaints. Try short, planned naps, break tasks into 15–30 minute blocks, and prioritize what must get done. For mobility, talk to a physical therapist about strengthening and balance exercises that fit your level. Occupational therapists can suggest small changes at home—grab bars, different utensils, or shoe choices—that reduce daily strain.
Mental health matters. Anxiety and depression are common with chronic illness. If you’re feeling low or foggy, tell your doctor. Counseling, peer groups, and low-impact exercise—walking, water therapy, gentle yoga—help more than you'd expect.
Medications can cause side effects like hair thinning or low phosphate levels. If a new drug seems to trigger hair loss or other odd symptoms, check resources on drug-induced effects and ask your provider about alternatives. Also be careful buying meds online: use licensed pharmacies and read guides on safe purchasing to avoid fake or unsafe products.
If you want deeper reading, our site has focused articles that are useful: guides on drug-induced hair loss, safe online pharmacy shopping, and practical info on meds used in neurological and autoimmune conditions. Bookmark them and bring questions to your next appointment—good notes help your team help you.
Finally, build your support: family, a specialist team, rehab professionals, and a pharmacist. Sclerosis changes life, but clear steps, honest talk with clinicians, and small daily adjustments make a big difference.
Living with sclerosis can be challenging, but maintaining an active social life is crucial for overall well-being. In my latest blog post, I offer tips to stay connected and engaged with friends and family. Some suggestions include using technology to keep in touch, joining support groups, and participating in accessible hobbies. I also emphasize the importance of self-care and open communication with loved ones. Don't let sclerosis hold you back from enjoying a fulfilling social life!
View Details