Myasthenia Gravis: Symptoms, Treatments, and Medication Insights
When your muscles tire too easily—like when you can’t hold up your eyelids, chew food, or even speak clearly—you might be dealing with myasthenia gravis, a chronic autoimmune disorder where the immune system attacks nerve-muscle connections. Also known as MG, it doesn’t affect the muscles themselves, but the signals that tell them to move. This breakdown happens because antibodies block or destroy acetylcholine receptors, the docking points on muscle cells that receive signals from nerves to trigger contraction. Without those signals, muscles don’t respond, even if they’re strong. It’s not muscle failure—it’s communication failure.
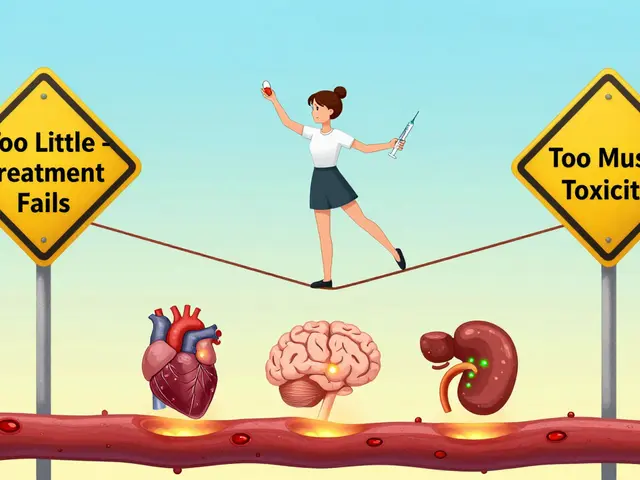
People with myasthenia gravis often notice symptoms get worse with activity and improve with rest. Common signs include drooping eyelids, double vision, trouble swallowing, slurred speech, and weakness in arms or legs. It’s not just fatigue—it’s a neurological signal dropout. The condition can start mild but may progress to affect breathing muscles, which is a medical emergency called myasthenic crisis. Treatment focuses on two goals: improving nerve-to-muscle signaling and calming the immune system. Pyridostigmine, a cholinesterase inhibitor, is often the first-line drug, helping acetylcholine stick around longer at the nerve endings. For longer-term control, doctors turn to immunosuppressants, like azathioprine or prednisone, to reduce the attack on receptors. Some patients benefit from thymectomy, a surgery to remove the thymus gland, which plays a role in triggering the autoimmune response.
What makes myasthenia gravis tricky is how it interacts with other medications. Certain antibiotics, beta-blockers, and even some anesthetics can make symptoms worse. That’s why knowing your full drug history matters. If you’re on multiple prescriptions, it’s not just about treating one condition—it’s about protecting your nerve-muscle connection. The same goes for supplements and over-the-counter meds. Even something as simple as magnesium can interfere with muscle function in MG patients.
The posts below cover real-world issues you might face if you or someone you know has myasthenia gravis. You’ll find guides on spotting dangerous drug interactions, managing side effects from immunosuppressants, and understanding how other conditions like liver disease or thyroid disorders can complicate treatment. There’s also advice on traveling with medications, reporting adverse reactions, and avoiding pharmacy errors that could put you at risk. This isn’t just theory—it’s practical info from people who’ve been through it, and the experts who help them stay safe.
Myasthenia gravis causes muscle weakness that worsens with use and improves with rest. Learn how AChR and MuSK antibodies drive the disease, why immunotherapy like IVIG, rituximab, and efgartigimod are changing treatment, and how thymectomy can lead to remission.
View Details