Pre-Surgery Preparation Checklist
Your Surgery Preparation Tracker
Enter your surgery date to receive personalized deadlines for all pre-operative tasks
Start by entering your surgery date to see your personalized schedule
Your Preparation Status
Next Steps:
Facing a procedure to clear a blocked pancreatic duct can feel overwhelming, but a solid preparation plan turns anxiety into confidence. Below is a step‑by‑step guide that walks you through everything you need to know before the operation, from medical tests to the day‑of‑hospital routine.
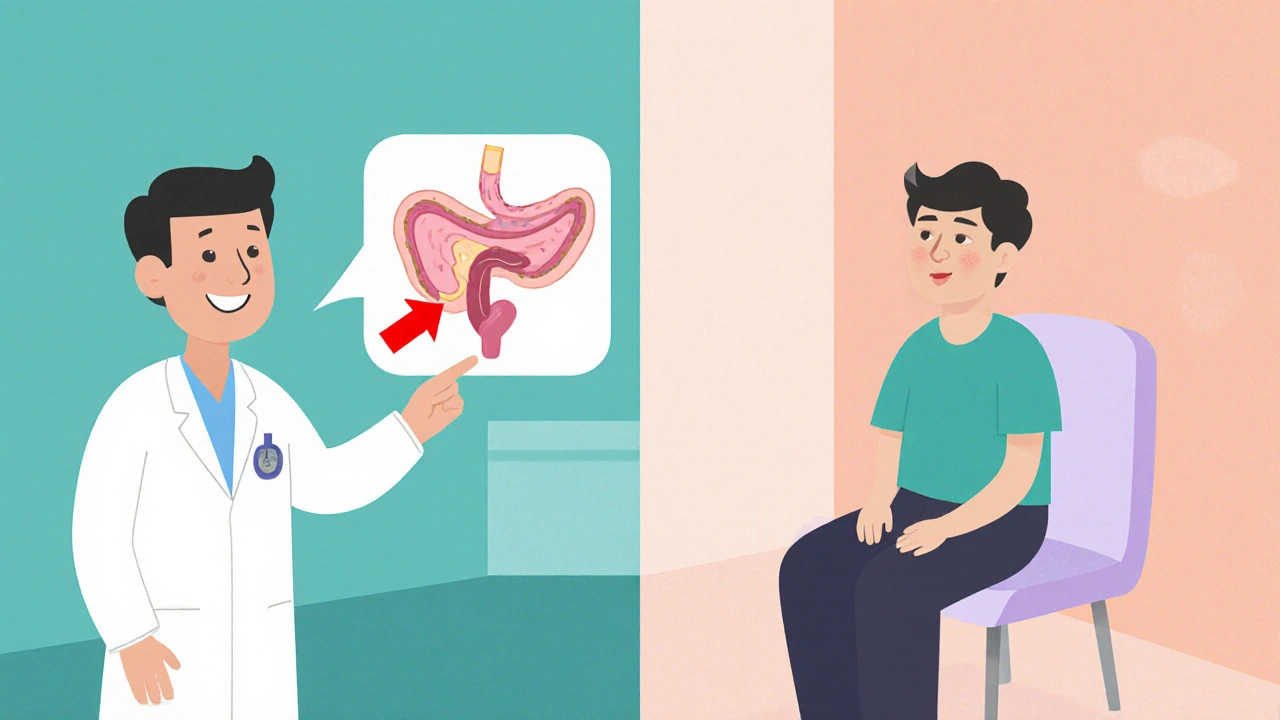
Understanding the Condition and the Surgery
Pancreatic duct blockage is a condition where the main conduit that carries digestive enzymes from the pancreas to the small intestine becomes narrowed or clogged, often leading to pain, inflammation, and digestive problems. When the blockage is severe, doctors may recommend surgery to restore flow and prevent further damage.
Two common surgical approaches are:
- Endoscopic Retrograde Cholangiopancreatography (ERCP) - a minimally invasive endoscopic technique that can place a stent to keep the duct open.
- Pancreaticojejunostomy - a more extensive operation that creates a new connection between the pancreas and the jejunum (part of the small intestine).
Whether you undergo an endoscopic procedure or a full‑scale surgery, the pre‑operative steps are quite similar.
Key Pre‑Surgery Tests and Their Purpose
Before the surgeon makes a final decision, several diagnostic tools help map the blockage and assess your overall health.
- CT scan - Provides detailed cross‑sectional images of the pancreas, showing the exact location and size of the obstruction.
- Blood tests - Measure liver enzymes, pancreatic enzymes (amylase, lipase), and markers of infection or inflammation.
- MRCP (Magnetic Resonance Cholangiopancreatography) - A non‑invasive MRI technique that visualises the pancreatic and bile ducts.
- Endoscopic ultrasound (EUS) - Allows the doctor to see inside the pancreas and take tissue samples if needed.
These tests give the surgical team a clear picture, reducing surprises on the operating table.
Medical Clearance: What Your Doctor Will Look For
Even if the imaging looks perfect, the anesthesiologist needs to be sure you can safely tolerate anesthesia.
- Heart health - an ECG and possibly a stress test.
- Lung function - a spirometry test if you have a history of smoking or respiratory issues.
- Kidney function - creatinine and eGFR levels to ensure medications are cleared properly.
- Medication review - especially blood thinners, diabetes meds, and any supplements.
Be prepared to share a complete medication list, including over‑the‑counter drugs and herbal products.
Day‑by‑Day Pre‑Op Checklist
| Time Frame | Action | Why It Matters |
|---|---|---|
| 4-6 weeks before | Schedule imaging (CT, MRCP) and blood work. | Provides the surgical roadmap and confirms fitness. |
| 2 weeks before | Stop smoking and limit alcohol. | Improves wound healing and reduces infection risk. |
| 7 days before | Begin NPO (nil per os) after midnight on the day of surgery. | Prevents aspiration while under anesthesia. |
| Day before | Take prescribed antibiotic prophylaxis if ordered. | Reduces postoperative infection rates. |
| Morning of surgery | Shower with antibacterial soap, wear loose‑fitting clothing. | Minimises skin bacteria that could enter the incision. |
| Arrival at hospital | Bring ID, insurance card, and a list of current medications. | Ensures smooth admission and accurate medication reconciliation. |
Nutrition and Lifestyle Adjustments
Good nutrition fuels recovery. A few weeks before surgery, aim for a balanced diet rich in protein, low‑fat, and easily digestible foods.
- Lean meats, fish, tofu, and eggs for protein.
- Steamed vegetables, peeled fruits, and low‑fiber grains to reduce pancreatic stimulation.
- Stay hydrated - at least 2 liters of water daily, unless your doctor advises otherwise.
Gentle exercise, such as walking or light stretching, keeps circulation strong without overtaxing the pancreas.
What to Pack for Your Hospital Stay
A short hospital stay (often 2-4 days) means you’ll need a few comfort items.
- Phone charger and a small speaker for music.
- Toothbrush, toothpaste, and lip balm.
- Loose‑fit pajamas and slippers.
- Any prescribed entertainment (books, puzzles).
Leave valuables at home - the hospital will keep personal belongings safe, but it’s best to travel light.
Day of Surgery: What Actually Happens
When you arrive, you’ll check in at the pre‑admission area. A nurse will verify your identity, confirm the NPO status, and place an IV line.
After a brief discussion with the anesthesiologist, you’ll be taken to the operating room. The surgery itself typically lasts 2-4 hours, depending on whether an endoscopic or open approach is used.
Post‑operative monitoring includes pain control, vital sign checks, and assessment of drain output if a surgical drain is placed.

Recovery Timeline and Early Warning Signs
Most patients feel comfortable enough to go home within a few days. Here’s a quick overview of what to expect:
- First 24 hours - Pain is managed with IV meds, you’ll start on a clear liquid diet.
- Days 2‑4 - Gradual advance to soft foods, light walking encouraged to prevent clots.
- Week 2 - Stitches (or staples) are removed, full diet resumed, and you may return to work depending on your job.
Call your surgeon or go to the emergency department if you notice any of the following:
- Fever above 38°C (100.4°F) that persists.
- Severe abdominal pain that doesn’t improve with prescribed meds.
- Redness, swelling, or pus around the incision.
- Yellowing of the skin or eyes (jaundice).
Common FAQs
How long should I be NPO before the surgery?
You must stop eating and drinking at midnight the night before the operation. Clear water is allowed if your surgeon says otherwise.
Can I take my regular pain medication before surgery?
Most pain meds, especially NSAIDs like ibuprofen, should be stopped 48 hours prior because they increase bleeding risk. Your doctor will give a specific list.
Is a hospital stay always required?
For endoscopic stenting, a same‑day discharge is often possible. Open pancreaticojejunostomy usually needs a 2‑ to 4‑day stay for monitoring.
What foods should I avoid after surgery?
Fatty, fried, and heavily spiced foods can overstimulate the pancreas. Stick to low‑fat proteins, cooked vegetables, and bland grains for the first few weeks.
When can I resume normal exercise?
Light walking can start the day after surgery. More vigorous activity, like running or heavy lifting, should wait at least 4-6 weeks, or until your surgeon clears you.
Final Thoughts
Preparing for surgery isn’t just about ticking boxes; it’s about giving your body the best chance to heal quickly and safely. Follow the checklist, keep communication open with your care team, and give yourself permission to rest and recover. With the right plan, you’ll move past the blockage and back to everyday life faster than you expect.

Ericka Suarez
21 October / 2025Listen up, folks-this whole pancreatic duct drama is a test of our grit. If you slap on that checklist and march into the OR like a true American, the odds tilt in your favor. Miss a step and you’re courting disaster, no excuses.