Steroid Comparison Calculator
Recommended Alternative
Enter values and click Calculate to see the equivalent dose and recommendation.
Quick Takeaways
- Medrol (methylprednisolone) is a medium‑potency oral corticosteroid commonly used for inflammation and immune suppression.
- Prednisone, dexamethasone, hydrocortisone, and budesonide are the most frequently considered alternatives.
- Potency, half‑life, and typical indications differ enough that the “best” substitute depends on the condition being treated.
- Side‑effect profiles are similar across steroids, but dosage and duration drive the risk level.
- Cost varies widely: generic prednisone is usually cheapest, while branded budesonide inhalers can be pricey.
What Is Medrol?
When you see the name Medrol is a brand‑name formulation of methylprednisolone, a synthetic glucocorticoid that mimics the body’s natural cortisol hormone. It’s taken orally as tablets, an injectable suspension, or a delayed‑release form. Medrol’s main job is to dampen inflammation and curb an overactive immune response.
Typical dosing ranges from 4mg to 48mg per day, depending on the severity of the disease. Because it’s more potent than hydrocortisone but less so than dexamethasone, many clinicians view it as a “middle‑ground” steroid.
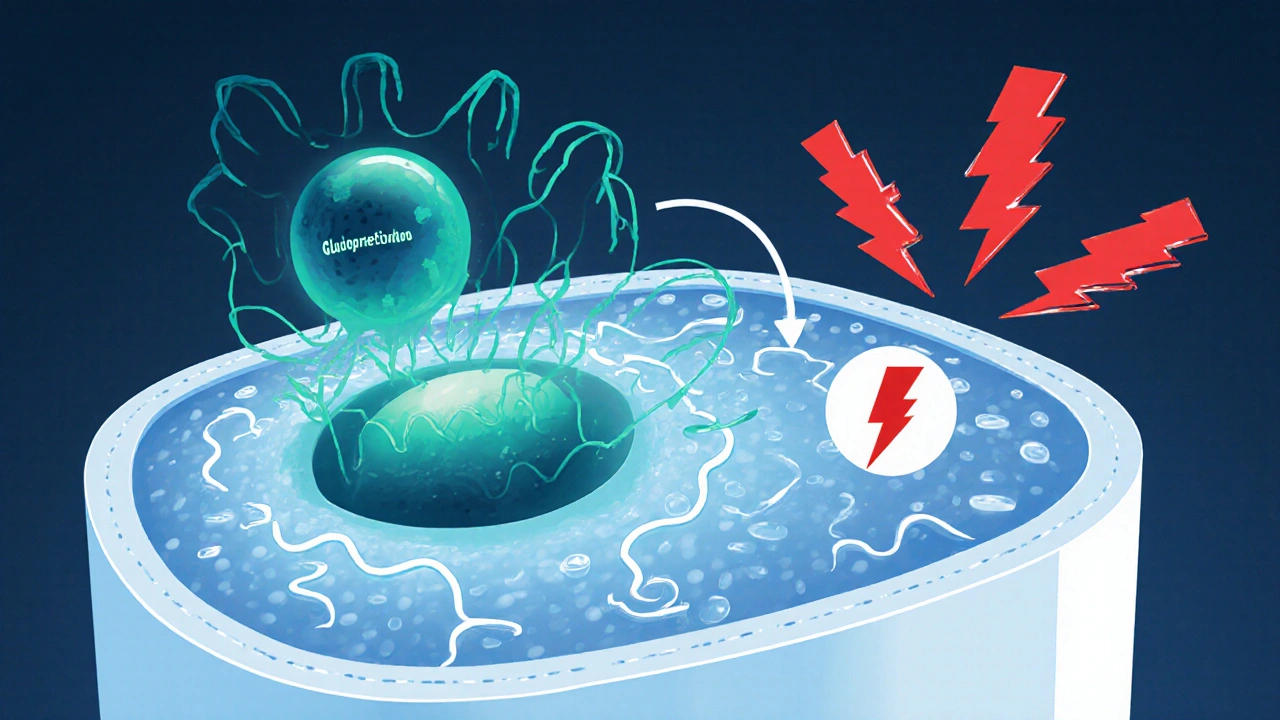
How Corticosteroids Work (The Big Picture)
Corticosteroids belong to a drug class that binds to glucocorticoid receptors inside cells. Once bound, they alter gene transcription, reducing the production of inflammatory messengers like prostaglandins and cytokines. This mechanism explains why a wide range of disorders-autoimmune diseases, allergic reactions, asthma exacerbations, and certain cancers-can be managed with steroids.
All steroids share this core action, but they differ in three practical dimensions:
- Potency - how strong the anti‑inflammatory effect is per milligram.
- Half‑life - how long the drug stays active in the bloodstream.
- Formulation - oral tablets, injectables, inhalers, topical creams, etc.
Understanding these variables helps you decide which alternative fits your needs.
Popular Alternatives to Medrol
Below are the five steroids most often considered when a doctor or patient wants to switch from Medrol.
Prednisone is a widely used oral glucocorticoid with about half the potency of methylprednisolone. It’s available in cheap generic tablets and is the go‑to option for chronic autoimmune conditions.
Dexamethasone is a high‑potency, long‑acting corticosteroid that’s roughly 6‑7 times stronger than prednisone. It’s favored for severe inflammatory crises, brain edema, and certain chemotherapy protocols.
Hydrocortisone is the synthetic version of the body’s natural cortisol, making it the lowest‑potency oral steroid. It’s often used for adrenal insufficiency or short‑term stress dosing.
Budesonide is a locally acting inhaled corticosteroid with high first‑pass metabolism, limiting systemic exposure. It’s the primary choice for asthma and chronic obstructive pulmonary disease (COPD) maintenance.
Betamethasone is a potent topical and injectable glucocorticoid, similar in strength to dexamethasone but often used for skin disorders. Its systemic use is limited due to strong potency.
Side‑Effect Landscape Across Steroids
Because all these drugs share the same receptor pathway, their adverse‑event profiles overlap. The biggest differences arise from dose, duration, and delivery method.
- Metabolic effects - increased blood sugar, weight gain, and fluid retention. Higher potency or longer half‑life (dexamethasone, betamethasone) heighten risk.
- Bone health - osteoporosis risk rises with cumulative dose; intermittent “pulse” regimens mitigate it.
- Immune suppression - higher doses open the door to infections, especially fungal and viral.
- Gastro‑intestinal irritation - all oral steroids can upset the stomach; concurrent PPIs are common prophylaxis.
- Psychiatric changes - mood swings, insomnia, even psychosis at high doses.
Inhaled budesonide sidesteps many systemic side effects because most of the drug is metabolized in the lung before entering circulation.
Comparison Table: Medrol vs. Alternatives
| Drug | Relative Potency* (per mg) | Half‑life (hrs) | Common Indications | Typical Oral Dose | Cost (US, generic/brand per month) |
|---|---|---|---|---|---|
| Medrol (methylprednisolone) | 1.0 (reference) | 18-36 | Rheumatoid arthritis, severe allergic reactions, asthma flare‑ups | 4mg-48mg daily | Generic $15‑$30; Brand $80‑$120 |
| Prednisone | 0.8 | 12-36 | Systemic lupus, COPD, skin conditions | 5mg-60mg daily | Generic $5‑$12 |
| Dexamethasone | 5-7 | 36-72 | Cerebral edema, chemotherapy adjunct, severe asthma | 0.5mg-10mg daily | Generic $8‑$20 |
| Hydrocortisone | 0.25 | 8-12 | Adrenal insufficiency, short‑term stress dosing | 10mg-100mg daily | Generic $4‑$10 |
| Budesonide (inhaled) | 1.5 (systemic exposure) | 2-4 (lung) | Asthma maintenance, COPD | 200‑800µg twice daily | Generic inhaler $30‑$70; Brand $150‑$250 |
| Betamethasone | 5-6 (topical/injectable) | 36-48 | Dermatitis, severe psoriasis, intra‑articular injections | 0.5mg-5mg intra‑articular/IV | Generic $12‑$25 |
*Potency is indexed to methylprednisolone (Medrol)=1.0 for easy comparison.

Choosing the Right Alternative: Decision Guide
Use the following quick decision tree to narrow down the best substitute for your situation.
- Is the goal systemic anti‑inflammation? If yes, stay with oral steroids (Prednisone, Dexamethasone, Hydrocortisone).
- For moderate potency and lower cost, Prednisone is usually the first pick.
- For high‑potency, short‑course needs (e.g., brain swelling), Dexamethasone shines.
- For adrenal insufficiency or very short bursts, Hydrocortisone mimics natural cortisol best.
- Do you need a lung‑focused therapy? If you’re treating asthma or COPD, an inhaled agent such as Budesonide reduces systemic exposure dramatically.
- Is the condition skin‑related or needing local injection? Betamethasone offers high topical potency without the systemic load of oral steroids.
- Is cost the dominant factor? Generic prednisone and hydrocortisone are the cheapest; brand‑name inhalers can be pricey but may be covered by insurance.
Practical Tips for Switching Steroids
Never change your medication on your own. Here are proven steps doctors follow when swapping one corticosteroid for another:
- Calculate equivalent dose using potency ratios (e.g., 4mg Medrol ≈ 5mg Prednisone).
- Taper if you’re moving to a longer‑acting steroid to avoid adrenal suppression.
- Monitor blood glucose especially in diabetics; high‑potency swaps can spike sugars.
- Watch for rebound inflammation during the first few days; a short overlap period (24‑48hrs) may be needed.
- Adjust supportive meds like calcium/vitaminD supplements to protect bone health.
Following these steps reduces the risk of withdrawal symptoms and keeps disease control steady.
Frequently Asked Questions
Can I use prednisone instead of Medrol for rheumatoid arthritis?
Yes. Prednisone provides comparable anti‑inflammatory effects at a slightly lower potency. Doctors often start with 5‑10mg daily and adjust based on disease activity. It’s also cheaper and widely covered by insurance.
What is the biggest safety concern when switching to dexamethasone?
Dexamethasone’s long half‑life can suppress the adrenal axis for several days after the last dose. A gradual taper or a short bridge with a shorter‑acting steroid (like prednisone) is recommended to prevent adrenal insufficiency.
Is inhaled budesonide safe for someone who’s already on oral steroids?
Adding budesonide can improve lung control while keeping systemic exposure low. However, doctors usually reduce the oral steroid dose once inhaled control is achieved, to limit cumulative side effects.
How long does it take for hydrocortisone to wear off after stopping?
Hydrocortisone’s short half‑life (8‑12hrs) means it clears from the bloodstream within 1‑2days. Nevertheless, the body’s natural cortisol production may need a few days to normalize, especially after high‑dose courses.
Why is betamethasone not commonly used systemically?
Its high potency makes systemic doses risky for side effects like severe hyperglycemia and mood changes. Clinicians reserve it for local applications (skin, joint injections) where the drug stays mostly where it’s needed.
Bottom Line
Medrol sits in the middle of the corticosteroid potency spectrum, making it a solid all‑rounder for many inflammatory conditions. When cost, specific organ targeting, or safety concerns come into play, alternatives such as prednisone, dexamethasone, hydrocortisone, budesonide, or betamethasone can be better fits. Use the comparison table and decision guide to match the drug to your clinical goal, and always involve a healthcare professional when adjusting doses.



peter derks
10 October / 2025Hey folks, great rundown on Medrol vs the other steroids! It’s super helpful to see potency, cost and typical uses side by side. If you’re new to steroid therapy, start by checking your doctor’s guidance and then use this table to compare options. Remember that the cheapest option might not be the most effective for your condition. Keep an eye on side‑effects especially with long‑term use. Stay proactive and keep asking your healthcare team about the best fit for you.