When you pick up a prescription, you might see two options: the familiar brand-name pill with the flashy logo, or a smaller, plain tablet with a different color and a much lower price tag. Which one should you choose? For most people, the answer isn’t about quality-it’s about understanding what really matters when it comes to your health and your wallet.
What Makes a Generic Drug the Same?
Generic drugs aren’t copies. They’re exact chemical twins of brand-name drugs. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration. That means if your doctor prescribes 20 mg of sertraline, whether you get Zoloft or its generic version, your body gets the same molecule that treats depression or anxiety.
The difference isn’t in what works-it’s in what doesn’t. Generics don’t contain the same inactive ingredients. That’s why a brand-name pill might be blue and oval, while the generic is white and round. These fillers, dyes, and binders don’t affect how the drug works. But they can affect how it looks, tastes, or even how easy it is to swallow.
Here’s the key: the FDA doesn’t approve generics unless they prove they deliver the same amount of medicine into your bloodstream at the same speed as the brand. This is called bioequivalence. Studies show the difference in absorption between brand and generic is usually less than 4%. That’s smaller than the natural variation your body has from day to day.
Why Are Generics So Much Cheaper?
Brand-name drugs cost a lot because the company had to pay for years of research, clinical trials, and marketing before they could sell it. That’s why a new drug might cost $400 a month. Once the patent expires-usually after 20 years-other companies can make the same drug without repeating all that expensive work.
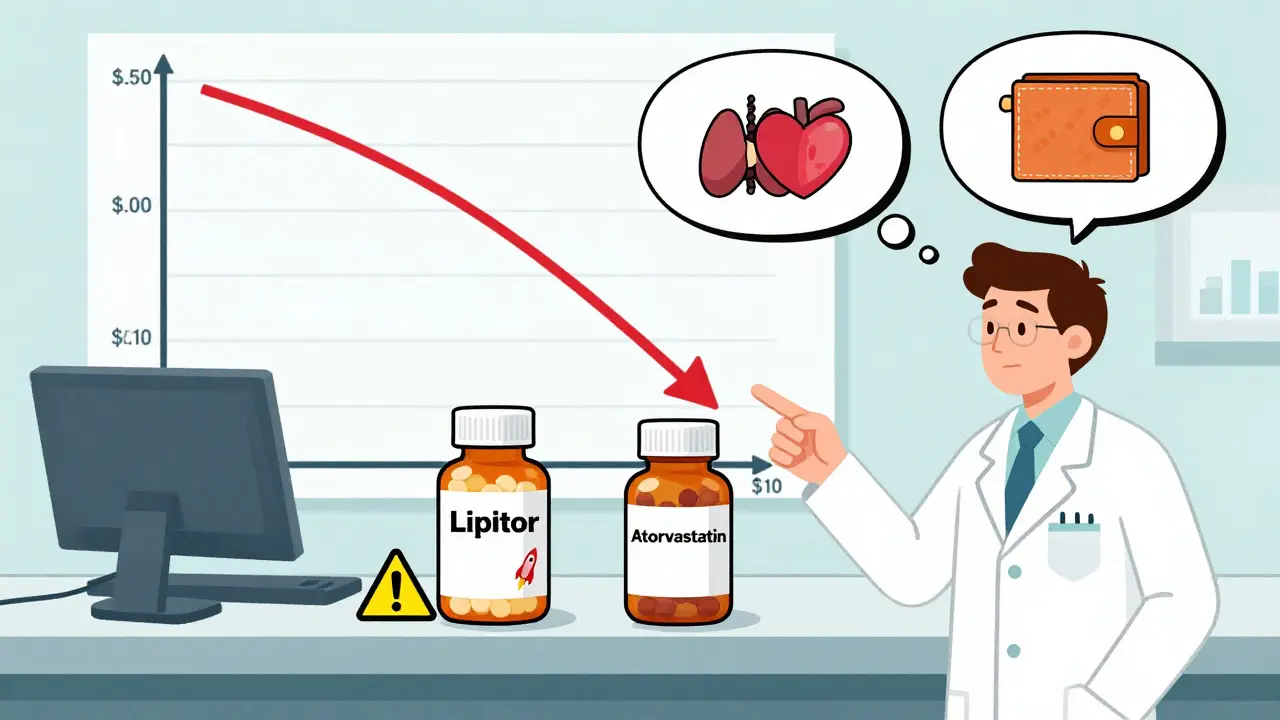
Generic manufacturers don’t need to run new clinical trials. They just need to prove their version behaves the same as the original. That cuts costs dramatically. On average, generics cost 80-85% less. For example:
- Atorvastatin (Lipitor generic): $0.10 per tablet vs. $4.50 for brand
- Sertraline (Zoloft generic): $4 for a 30-day supply vs. $400 for brand
- Pregabalin (Lyrica generic): $15 per month vs. $650 for brand
Over the last decade, generics saved the U.S. healthcare system over $1.67 trillion. That’s $265 saved per person every year. That’s not a small amount-it’s the difference between taking your medicine or skipping doses because you can’t afford it.
When Should You Stick With the Brand?
Most of the time, generics work just as well. But there are exceptions. For drugs with a narrow therapeutic index, even tiny changes in blood levels can matter. These include:
- Levothyroxine (for thyroid conditions)
- Warfarin (a blood thinner)
- Phenytoin and carbamazepine (for seizures)
In these cases, switching between different generics-or even between brand and generic-can cause your levels to shift. That’s why 28 states require doctors to specify “dispense as written” for these drugs. If you’re on one of these, consistency matters. Stick with the same manufacturer if possible. If your pharmacy switches your generic, ask your pharmacist to notify you. Your doctor might need to check your blood levels more often.
Some complex delivery systems also pose challenges. Inhalers like Advair Diskus, patches, or extended-release capsules rely on how the drug is released over time. A 2016 study found 12% of patients switching from Advair to a generic inhaler had trouble using the device properly-even though the medicine inside was the same. The difference wasn’t in the drug. It was in the device.
What Do Real Patients Say?
Over 15,000 patient reviews on Drugs.com show 82% satisfaction with generics versus 85% for brand-name drugs. That’s a tiny gap. But the complaints aren’t about effectiveness-they’re about confusion.
People report:
- Getting a different-looking pill and thinking it’s the wrong medication
- Switching between generic manufacturers and noticing a change in how they feel
- Being scared to switch because they’ve always taken the brand
One common issue is with bupropion XL (Wellbutrin). Some patients report reduced effectiveness when switching to generic versions. The FDA issued a warning in 2012 about certain extended-release formulations not being fully bioequivalent. That’s why some doctors still prescribe the brand for depression treatment-even though most generics work fine.
On Reddit’s r/PersonalFinance, 93% of people who switched to generics said the main reason was cost. One user wrote: “I was skipping my pills because the brand cost $700/month. The generic is $18. I haven’t missed a dose since.”
How to Make the Switch Safely
If your doctor hasn’t told you otherwise, you’re allowed to get the generic. But here’s how to make sure it goes smoothly:
- Ask your pharmacist: “Is this a new manufacturer?” If the pill looks different, ask them to confirm it’s the same drug.
- Use the FDA’s Drugs@FDA database to look up your medication and see which generics are approved and rated as equivalent (they’ll say “AB”).
- If you’re on a narrow therapeutic index drug, ask your doctor if you should stay on one brand or manufacturer.
- Keep a list of your medications and the pill appearance (color, shape, imprint). Take a photo if needed.
- Don’t switch brands or generics without talking to your doctor or pharmacist-especially for heart, thyroid, or seizure meds.
Pharmacists are trained to help with this. A 2022 survey found that 68% of patients were nervous about generics at first. After a 5-minute explanation from their pharmacist, 89% were comfortable continuing with them.

What’s Changing in 2026?
The Inflation Reduction Act of 2022 lets Medicare negotiate prices for 10 high-cost drugs starting in 2026. That means more brand-name drugs will face pressure to lower prices-or face competition from generics. More patents are expiring too. Between 2023 and 2027, $260 billion worth of brand-name drugs will lose exclusivity.
At the same time, the FDA is working on better rules for complex generics-like inhalers, eye drops, and injectables. Right now, only 35% of off-patent complex drugs have generic versions. That’s changing.
But there’s a warning: 78% of the active ingredients in generics come from India and China. Supply chain issues can cause shortages. That’s why some patients get the same generic one month, then a different one the next. It’s not about quality-it’s about availability.
Final Advice: Trust the Science, Not the Brand
Brand-name drugs aren’t better. They’re just more expensive. The FDA holds generics to the same standards. The data doesn’t lie: 98.5% of the time, generics work just as well.
Cost is the real issue. If you’re skipping doses because your medicine is too expensive, switching to a generic could save your life. One study found that patients on generics had 22% better adherence than those on brand-only drugs.
Don’t let the shape, color, or price tag fool you. What matters is whether the medicine works. For most people, the generic does. For a small number, the brand-or a consistent generic-is necessary. Talk to your doctor. Ask your pharmacist. And remember: your health isn’t about the logo on the bottle. It’s about what’s inside.

shivani acharya
21 January / 2026So let me get this straight - the FDA says generics are ‘exact chemical twins’ but 78% of the active ingredients come from India and China, where regulatory oversight is basically a suggestion? 🤔 I’ve seen pills that look like they were manufactured in a garage with a 3D printer and a dream. My cousin took a generic version of her thyroid med and ended up in the ER because her body decided to revolt. Coincidence? Or just the price of ‘saving’ $395 a month? I’m not anti-generic - I’m pro-not-dying.