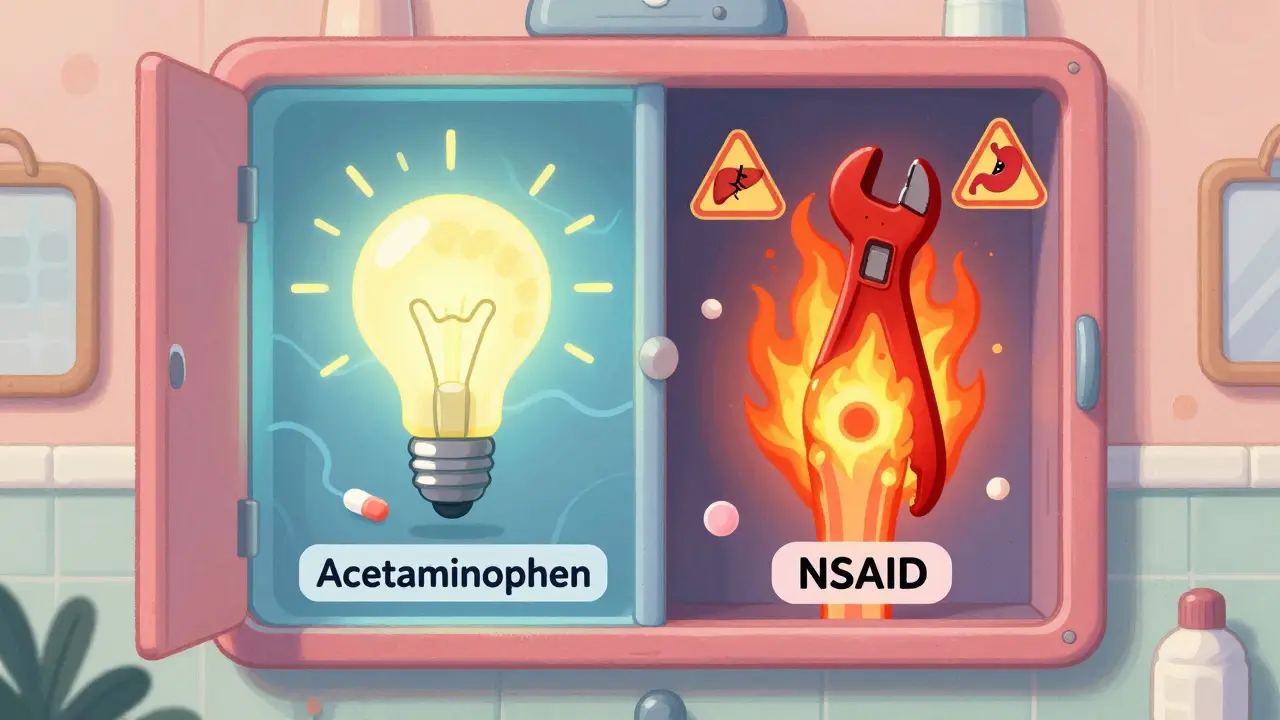
What’s the real difference between acetaminophen and NSAIDs?
You’ve got a headache. Your knee is throbbing after gardening. Maybe you’re nursing a fever. You reach for the medicine cabinet. But which pill do you grab? Acetaminophen or an NSAID? It’s not just about brand names like Tylenol or Advil - it’s about what’s actually happening inside your body. These two types of pain relievers work in completely different ways, and choosing the wrong one can mean less relief… or worse, real harm.
How acetaminophen actually works (and where it falls short)
Acetaminophen, the active ingredient in Tylenol and countless generic brands, doesn’t touch inflammation. That’s the big one. It works mainly in your brain and spinal cord, raising your pain threshold. Think of it like turning down the volume on pain signals, not fixing the source. It’s great for headaches, mild back pain, and fever. In fact, about 70% of people with migraines find relief with it, according to Mayo Clinic data. It’s also the only OTC painkiller recommended for kids under 12 and pregnant women - because it doesn’t irritate the stomach or affect blood clotting like NSAIDs do.
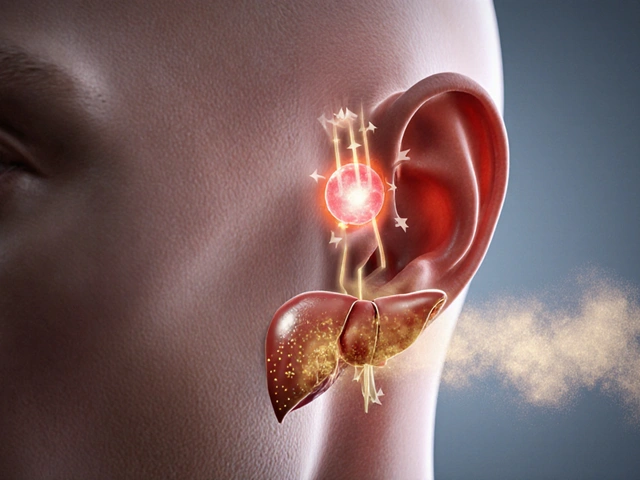
But here’s the catch: acetaminophen has a razor-thin safety margin. The official max daily dose is 4,000 milligrams - that’s eight extra-strength tablets. But Harvard Health recommends staying under 3,000 mg to be safe. Why? Because liver damage can happen even within the "safe" range, especially if you drink alcohol regularly, have existing liver issues, or accidentally take it from multiple sources. Nearly 40% of acetaminophen-related liver injuries come from people combining cold meds, sleep aids, or prescription painkillers that also contain acetaminophen. The FDA now requires bright red warnings on every bottle because of this. In 2022, the CDC reported over 15,000 hospitalizations in the U.S. alone from accidental overdose.
How NSAIDs work - and why they’re better for swelling and joint pain
NSAIDs - that’s nonsteroidal anti-inflammatory drugs - include ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin. These drugs block enzymes called COX-1 and COX-2 all over your body. That means they reduce not just pain and fever, but also inflammation - the redness, heat, and swelling that come with arthritis, sprains, or menstrual cramps. That’s why they’re often the go-to for knee or hip osteoarthritis. Studies show NSAIDs reduce pain scores by 30-50% in these cases, while acetaminophen only helps by 10-20%. For muscle strains, tendonitis, or a bad case of period pain, NSAIDs are usually the winner.
But they come with trade-offs. Taking NSAIDs long-term increases your risk of stomach ulcers by 2-4% per year. They can also raise blood pressure and, in high doses or with pre-existing heart conditions, increase the risk of heart attack or stroke. The FDA has required warning labels on all OTC NSAIDs since 2015. Naproxen tends to carry slightly lower cardiovascular risk than ibuprofen, according to 2021 research in the European Heart Journal. And if you take NSAIDs often, it’s smart to take them with food or even pair them with a stomach-protecting drug like famotidine.

Which one should you pick - and when?
There’s no one-size-fits-all answer. It depends on what’s hurting you.
- For a simple headache, fever, or toothache? Start with acetaminophen. It’s gentler on your stomach and safe during pregnancy.
- For arthritis, swollen joints, a sprained ankle, or period cramps? Go with an NSAID. You’ll feel the difference because it’s fighting the inflammation, not just masking the pain.
- For chronic back pain? Try acetaminophen first - it’s safer for long-term use if you don’t have liver issues. If it doesn’t help after a few days, switch to an NSAID for a short burst.
- For kids? Only acetaminophen or ibuprofen are approved. Always check the weight-based dosing chart. Never give aspirin to children - it can cause Reye’s syndrome, a rare but deadly condition.
And here’s a pro tip: you don’t have to pick just one. Harvard Health and other experts say combining a low dose of acetaminophen with a low dose of an NSAID can give you better pain relief than either alone - and let you use less of each, cutting down on side effects. Just make sure you’re not doubling up on acetaminophen from another product.
The hidden dangers you’re probably ignoring
Most people think OTC means "harmless." That’s dangerous thinking.
With acetaminophen, the biggest risk isn’t taking too much at once - it’s taking a little extra every day. Cold medicine, sleep aids, prescription opioids like hydrocodone - they all often contain acetaminophen. You might think you’re only taking two Tylenol tablets, but if you also took a nighttime cold pill, you’ve already hit 3,000 mg before noon. That’s why the FDA changed labeling rules in 2011: every bottle now has a bold warning about liver damage.
With NSAIDs, the danger builds slowly. One pill a day for weeks might seem fine. But over time, they wear down your stomach lining. People don’t realize they’re developing ulcers until they start vomiting blood or pass black, tarry stools. And if you have high blood pressure, heart disease, or kidney problems, NSAIDs can make those worse. The American Heart Association now advises people with established heart disease to avoid NSAIDs unless absolutely necessary.

Cost, availability, and what’s on the horizon
Both types are cheap. Generic acetaminophen costs about 3 to 5 cents per 500mg tablet. Ibuprofen runs 4 to 7 cents per 200mg tablet. You can buy them at any pharmacy, grocery store, or gas station - no prescription needed.
Market data shows Americans spend about $1.5 billion a year on OTC pain relievers. Acetaminophen still leads with 40% of sales, followed by ibuprofen at 35% and naproxen at 25%. But the real story isn’t sales - it’s safety awareness. More people are learning to read labels and ask pharmacists questions. That’s good.
Research is moving forward. The NIH is funding 17 clinical trials as of late 2023 to find new pain treatments that avoid the risks of both acetaminophen and NSAIDs. But for now, these two remain the backbone of OTC pain relief. Experts from Harvard, Mayo Clinic, and Yale all agree: they’re not going away anytime soon. You’ll still be reaching for them in 2030 - if you use them wisely.
What to do if pain won’t go away
If you’ve tried both acetaminophen and NSAIDs at full recommended doses for a few days and your pain hasn’t improved, it’s time to see a doctor. Chronic pain isn’t something to tough out with pills. It could be a sign of something deeper - a pinched nerve, an autoimmune issue, or even something unrelated to inflammation. Don’t keep increasing your dose. Don’t mix more drugs. Get help.
Can I take acetaminophen and ibuprofen together?
Yes, you can safely take acetaminophen and ibuprofen together if you follow the correct doses for each. Many doctors recommend this combination because they work in different ways - acetaminophen targets pain signals in the brain, while ibuprofen reduces inflammation. Taking both can give you better pain relief than either alone, and it lets you use lower doses of each, reducing side effects. Just make sure you’re not taking any other meds that contain acetaminophen, and don’t exceed 3,000 mg of acetaminophen per day or 1,200 mg of ibuprofen.
Is acetaminophen safer than NSAIDs for the stomach?
Yes, acetaminophen is much safer for your stomach. NSAIDs like ibuprofen and naproxen block protective enzymes in the stomach lining, which can lead to ulcers, bleeding, or perforation - especially with regular use. Studies show NSAID users have a 2-4% annual risk of developing stomach ulcers. Acetaminophen users have less than a 0.5% risk. That’s why acetaminophen is the first choice for people with a history of stomach problems, older adults, or those on blood thinners.
Why can’t I give aspirin to my child?
Aspirin can cause Reye’s syndrome in children and teenagers, especially when taken during viral infections like the flu or chickenpox. Reye’s syndrome is rare but can cause sudden brain and liver damage. It’s been almost eliminated in countries where parents avoid giving aspirin to kids. Always use acetaminophen or ibuprofen for children’s fever or pain. Never give aspirin to anyone under 18 unless a doctor specifically prescribes it for a rare condition like Kawasaki disease.
Which NSAID is safest for the heart?
Among OTC NSAIDs, naproxen appears to carry the lowest cardiovascular risk. A 2021 study in the European Heart Journal found that naproxen didn’t significantly raise the risk of heart attack or stroke at standard doses, unlike ibuprofen, which increased risk by 10-50% with long-term use. If you have heart disease or high blood pressure and need an NSAID, naproxen is generally the preferred choice - but still only for short-term use. Always talk to your doctor first.
Can I drink alcohol while taking acetaminophen?
It’s not safe. Even moderate drinking - like one or two drinks a day - can increase your risk of liver damage when combined with acetaminophen. The liver processes both alcohol and acetaminophen, and together they create toxic byproducts that can kill liver cells. If you drink regularly, limit acetaminophen to no more than 2,000 mg per day, and only when absolutely necessary. If you have liver disease, avoid it entirely. Better yet, talk to your pharmacist before mixing any meds with alcohol.
What’s the best way to avoid overdosing on acetaminophen?
Always read every medicine label - even the ones you think are "just for colds" or "just to help me sleep." Many combination products like NyQuil, Excedrin, and prescription painkillers contain acetaminophen. Keep a list of everything you’re taking and check the active ingredients. Never take more than one product with acetaminophen at the same time. Set a daily limit of 3,000 mg or less, and never exceed 4,000 mg under any circumstances. If you’re unsure, ask your pharmacist to check your meds.