Combining blood thinners with common pain relievers like ibuprofen or naproxen isn’t just a bad idea-it’s a dangerous mix that can send you to the hospital for life-threatening bleeding. This isn’t theoretical. It’s backed by hard data from a major study of over 51,000 people, and the numbers don’t lie.
What’s at Stake: Bleeding You Can’t See Coming
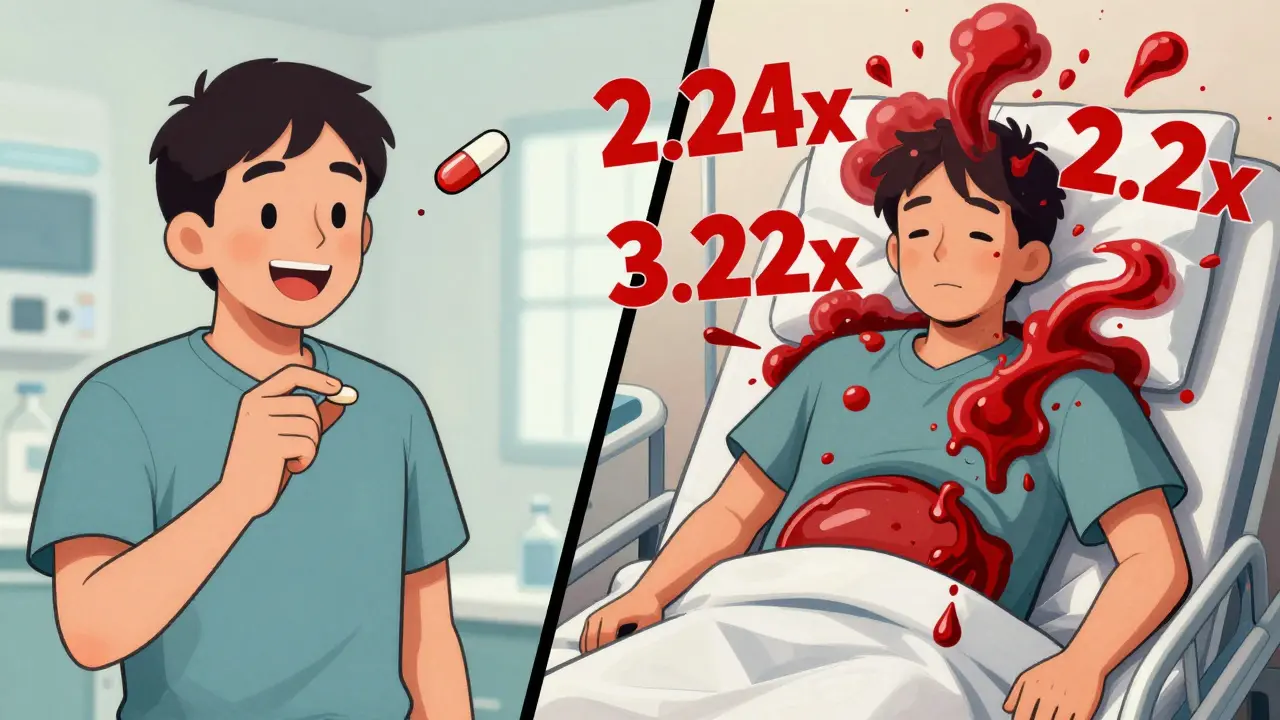
People on blood thinners-whether it’s warfarin, apixaban, rivaroxaban, or another anticoagulant-are already at higher risk for bleeding. Add an NSAID like ibuprofen, naproxen, or diclofenac, and that risk doesn’t just go up a little. It explodes. A 2024 study from Aarhus University Hospital tracked patients on anticoagulants for venous thromboembolism over a decade. The results? Taking an NSAID alongside a blood thinner more than doubled the chance of being hospitalized for bleeding. That’s not a small increase. That’s a red flag. The bleeding doesn’t just happen in your stomach. The study found higher risks across multiple areas:- Gastrointestinal bleeding: 2.24 times more likely
- Intracranial bleeding (brain): 3.22 times more likely
- Pulmonary bleeding (lungs): 1.36 times more likely
- Urinary tract bleeding: 1.57 times more likely
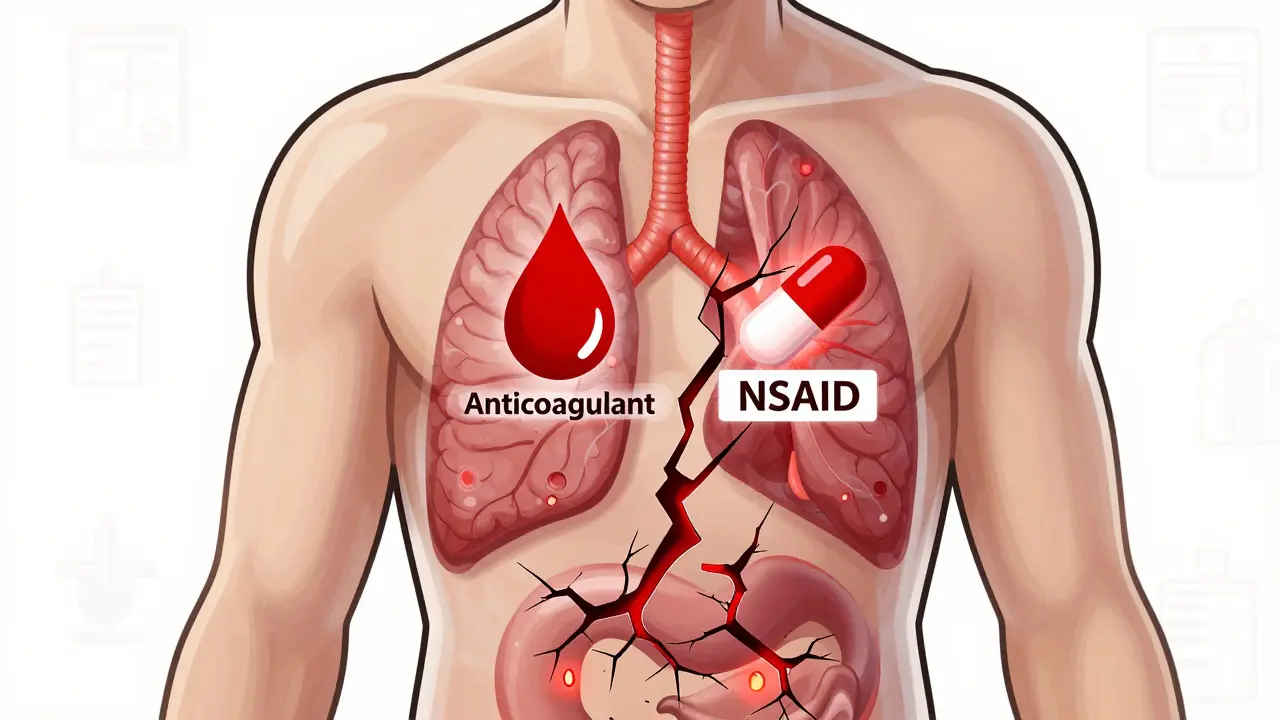
Why This Happens: Two Ways Your Blood Stops Clotting
Blood thinners work by slowing down your body’s ability to form clots. Warfarin blocks vitamin K-dependent clotting factors. DOACs like apixaban or dabigatran target specific proteins in the clotting cascade. They’re effective-but they leave you vulnerable. NSAIDs do something different, but just as dangerous. They block cyclooxygenase (COX) enzymes, especially COX-1. That’s the enzyme that helps protect your stomach lining and lets platelets stick together to form clots. When COX-1 is shut down:- Your stomach lining becomes more prone to ulcers and tears
- Your platelets can’t clump properly to stop bleeding
Not All NSAIDs Are Created Equal
You might think, “I just take ibuprofen occasionally-it’s OTC, so it’s safe.” But the data says otherwise. The same 2024 study ranked NSAIDs by how much they increased bleeding risk:- Naproxen: 4.1 times higher risk
- Diclofenac: 3.3 times higher risk
- Ibuprofen: 1.79 times higher risk
It Doesn’t Matter Which Blood Thinner You’re On
Some people assume that newer anticoagulants (DOACs) are safer than warfarin. That’s true in some ways-but not when NSAIDs are involved. The Danish study found no difference in bleeding risk between warfarin and DOACs when NSAIDs were added. Whether you’re on Eliquis, Xarelto, or Coumadin, combining any of them with an NSAID puts you at the same elevated risk. There’s no “safer” blood thinner in this scenario.What You Should Do Instead
If you’re on a blood thinner and need pain relief, you have better options.- Acetaminophen (Tylenol): This is the go-to alternative. It doesn’t affect platelets or stomach lining. It’s not perfect-too much can hurt your liver-but at recommended doses, it’s the safest choice for pain or fever while on anticoagulants.
- Physical therapy and heat/cold therapy: For arthritis or muscle pain, these are effective and risk-free. A heating pad, ice pack, or guided stretching can do more than you think.
- Topical NSAIDs: Gels or patches like diclofenac gel applied to the skin deliver very little into the bloodstream. They’re a better option than pills, though still not risk-free. Talk to your doctor before using them.
Why People Don’t Realize the Danger
Many patients don’t think of OTC painkillers as “real drugs.” They’ll say, “I only take ibuprofen when I have a headache,” or “I use naproxen for my back pain once a week.” But that’s enough. The Danish study showed even short-term NSAID use-just a few days-significantly raised bleeding risk. And because these drugs are sold over the counter, many people don’t tell their doctors they’re taking them. Doctors need to ask. Specifically. Not just, “Are you on any medications?” but, “Do you take any pain relievers-even once in a while? Including ibuprofen, naproxen, or aspirin?”What If You Absolutely Need an NSAID?
Sometimes, there’s no alternative. Maybe you have acute gout or a severe inflammatory flare. In those rare cases:- Use the lowest effective dose
- Take it for the shortest time possible
- Don’t assume a proton pump inhibitor (like omeprazole) protects you fully-the study showed bleeding risk still rose in the brain, lungs, and urinary tract, even with stomach protection
The Bigger Picture: A Growing Public Health Problem
About 3 to 6 million Americans take blood thinners. In the U.S. alone, roughly 30 billion OTC ibuprofen tablets are sold each year. That’s a massive overlap. The American College of Cardiology says this combination is one of the most common-and dangerous-drug interactions in clinical practice. And it’s only getting worse as more people live longer with conditions like atrial fibrillation and arthritis. Health systems are starting to respond. Some electronic health records now flag patients on anticoagulants who are prescribed NSAIDs. Pharmacists are being trained to intervene. But until everyone knows the risk, people will keep getting hurt.Bottom Line: Skip the NSAID. Choose Safer Pain Relief.
If you’re on a blood thinner, acetaminophen is your best friend for pain. Physical methods like heat, ice, or stretching help too. NSAIDs-even the ones you buy without a prescription-are not worth the risk. This isn’t about being overly cautious. It’s about survival. The numbers are clear: combining these drugs multiplies your chance of bleeding-and that bleeding can happen anywhere: in your brain, your lungs, your gut. You won’t always see it coming. But your doctor can help you avoid it.Can I take ibuprofen with warfarin if I only use it once in a while?
No. Even occasional use of ibuprofen while on warfarin increases your bleeding risk by nearly 80%. The Danish study showed that even short-term use-just a few days-significantly raises the chance of hospitalization for bleeding. There’s no safe threshold. Acetaminophen is the safer alternative.
Are newer blood thinners safer than warfarin when combined with NSAIDs?
No. The 2024 study found no difference in bleeding risk between warfarin and DOACs (like apixaban or rivaroxaban) when NSAIDs were taken. The danger comes from the NSAID, not the type of blood thinner. All anticoagulants interact dangerously with NSAIDs.
What about aspirin? Is it safe with blood thinners?
Aspirin is an NSAID and also an antiplatelet drug. It’s not safe with other blood thinners unless specifically prescribed by your doctor for heart protection. Even low-dose aspirin increases bleeding risk when combined with anticoagulants. Never take aspirin with a blood thinner without medical approval.
Can I use a topical NSAID gel instead of pills?
Topical NSAIDs (like diclofenac gel) deliver much less drug into the bloodstream, so they’re less risky than oral forms. But they’re not risk-free. Some absorption still occurs, and bleeding risk isn’t eliminated. Talk to your doctor before using them, especially if you’re on a strong anticoagulant.
Should I stop taking my NSAID if I start a blood thinner?
Yes-unless your doctor specifically says otherwise. If you’re starting a blood thinner, review all your medications with your provider. NSAIDs should be discontinued unless there’s no other option. If pain persists, switch to acetaminophen or non-drug therapies like heat, ice, or physical therapy.
Does taking a stomach protector (like omeprazole) make NSAIDs safe with blood thinners?
No. While proton pump inhibitors reduce the risk of stomach ulcers, they don’t protect against bleeding in other areas like the brain, lungs, or urinary tract. The Danish study confirmed that even with stomach protection, the overall risk of bleeding remained significantly higher. The problem isn’t just your stomach-it’s your entire clotting system.

Liam Crean
18 February / 2026I never realized how dangerous this combo was until my uncle ended up in the ER. He was taking ibuprofen for his arthritis and warfarin for AFib. Thought it was harmless. Turns out, he had a GI bleed they didn't catch until he passed out at the grocery store. Now he's on Tylenol and a heating pad. Best decision he ever made.