Stem Cell Transplant: A Simple, Straight‑forward Guide
If you or a loved one has been told you need a stem cell transplant, the first reaction is usually a mix of hope and fear. That’s normal. This page breaks down the basics, why doctors recommend it, what actually happens, and how to handle life after the procedure—all in plain language.
What Is a Stem Cell Transplant?
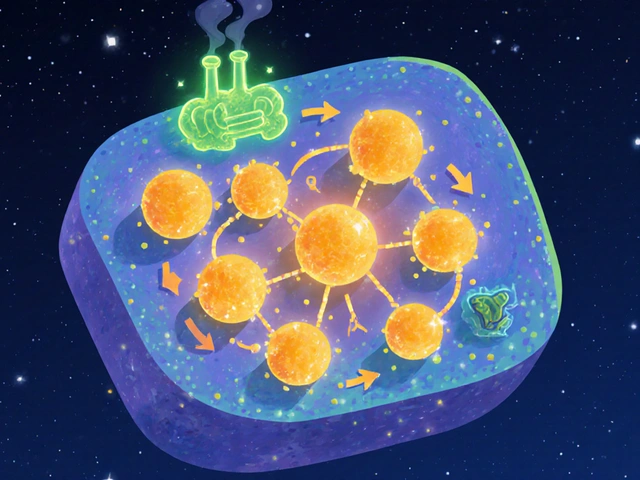
In a nutshell, a stem cell transplant (often called a bone marrow transplant) replaces damaged or diseased blood‑forming cells with healthy ones. Doctors collect stem cells from your own body (autologous), a matching donor (allogeneic), or from umbilical cord blood. Those cells are then infused into your bloodstream, where they travel to the bone marrow and start making new blood cells.
Common reasons for a transplant include blood cancers like leukemia, certain lymphomas, and severe aplastic anemia. It can also be used for some genetic disorders and immune system problems.
Who Is a Good Candidate?
Eligibility isn’t a one‑size‑fits‑all. Your doctor will look at age, overall health, organ function, and the type of disease you have. Younger patients usually tolerate the intense chemotherapy or radiation that prepares the body better, but older adults can still qualify if they’re in good shape.
Key factors include:
- Enough healthy organ function (heart, lungs, kidneys)
- Ability to handle high‑dose chemo or radiation
- A suitable donor match, if you need an allogeneic graft
- No active infections that could flare up during treatment
If you’re unsure, ask your doctor for a clear list of the tests they use to decide.
Preparing for the Procedure
Preparation is the part most people dread, but knowing what to expect makes it easier. First, you’ll go through a conditioning regimen—high‑dose chemo, radiation, or both—to wipe out the faulty cells and make space for the new stem cells. This can cause nausea, fatigue, and a drop in blood counts, so doctors often give anti‑nausea meds and growth factors.
While you’re in the hospital, nurses will draw blood for the stem cell collection. If you’re donating, the process is called apheresis and takes a few hours. For a donor match, a quick cheek swab or blood test determines compatibility.Practical tips:
- Stock up on easy‑to‑digest foods (soups, smoothies) for after the conditioning.
- Arrange transportation and a caregiver for the first weeks.
- Ask about medication schedules—missing a dose can affect engraftment.
Day of Transplant and Immediate Recovery
On transplant day, the stem cells are infused through a central line—think of it like a slow IV. The infusion itself feels like a regular blood draw and usually takes 30‑60 minutes. After that, you’ll stay in a protected hospital room until your new cells start working, which is called engraftment.
Engraftment typically occurs 10‑30 days post‑transplant. During this window, watch for fever, bleeding, or infections—your immune system will be very weak. Doctors will give antibiotics, antivirals, and antifungals to keep you safe.
Long‑Term Recovery and Follow‑Up
Once you’re out of the hospital, the real work begins. You’ll need regular blood tests to track cell counts and organ health. Physical activity should start slow—short walks, gentle stretching, and gradually building up strength. Nutrition matters, too; protein‑rich foods help tissue repair.
Potential long‑term side effects include graft‑versus‑host disease (GVHD) if you received donor cells, hormone changes, or fatigue that lasts months. Most issues are manageable with medication and lifestyle tweaks, but keep an eye on any new symptoms and report them promptly.
Emotional health is just as important. It’s normal to feel anxious or depressed after a big procedure. Support groups, counseling, or talking with friends who’ve been through it can make a huge difference.
Quick FAQ
How long does the whole process take? From diagnosis to full recovery, you’re looking at 6‑12 months, depending on the disease and your body’s response.
Can I work during recovery? Many patients return to light office work after 2‑3 months, but it varies. Listen to your body.
What’s the success rate? For many leukemias, 5‑year survival rates are over 50‑70% with a matched donor. Your doctor can give you numbers specific to your condition.
Stem cell transplants can feel overwhelming, but breaking the journey into bite‑size steps helps. Keep a list of questions, lean on your care team, and remember that millions have walked this path and come out the other side. If you stay informed and proactive, you give yourself the best shot at a smooth recovery.
A detailed guide to treatment options for chromosome-positive lymphoblastic leukemia, covering targeted drugs, chemotherapy, transplant, and emerging immunotherapies.
View Details