Opioid Overdose Recognition Quiz
Test Your Knowledge: Recognize the Signs
Question 1 of 5
A person is lying on the floor. They don't respond when you shake them. Their breathing is slow and shallow. Their lips and fingernails are blue. What should you do first?
Someone you care about stops breathing. Their lips are blue. They don’t respond when you shake them. Their skin is cold and clammy. You hear a gurgling sound - like they’re drowning in their own saliva. This isn’t a nightmare. It’s an opioid overdose. And it can kill in under five minutes.
If you’ve ever wondered what to do when someone overdoses, you’re not alone. Most people don’t know the signs until it’s too late. But here’s the truth: opioid overdose is preventable. You don’t need to be a doctor. You don’t need special training. You just need to know what to look for - and what to do next.
What Happens During an Opioid Overdose
Opioids - whether prescription painkillers like oxycodone, illegal heroin, or deadly synthetic drugs like fentanyl - work by slowing down your brain’s breathing signals. When someone takes too much, those signals shut off completely. The person stops breathing. Oxygen stops reaching the brain. Brain cells begin to die within minutes.
This isn’t just about drugs people take recreationally. Many overdoses happen to people who were prescribed opioids after surgery or for chronic pain. Others take pills bought off the street, thinking they’re Xanax or Percocet - only to find out they contain fentanyl. The CDC reports that in 2023, 81% of all drug overdose deaths in the U.S. involved opioids. Fentanyl, which is 50 to 100 times stronger than morphine, is now the main driver of these deaths.
The Three Classic Signs of an Opioid Overdose
You don’t need a medical degree to spot an overdose. Look for these three key signs - often called the opioid overdose triad:
- Unresponsive or unconscious - The person won’t wake up, even when you shake them hard or shout their name. They may slump over, head drooping, eyes closed.
- Slow, shallow, or stopped breathing - Their chest isn’t moving. You hear gasping, snoring, or gurgling - not normal breaths. Sometimes they take only one breath every 10 seconds.
- Pinpoint pupils - Their pupils are tiny, like pinpricks, even in dim light. (Note: Not everyone has this sign, so don’t wait for it.)
Other warning signs include:
- Blue, purple, or gray lips and fingernails (cyanosis)
- Cold, clammy, or pale skin
- Limp body - like a ragdoll
- Choking or gurgling sounds
- Extreme drowsiness or inability to stay awake
Some people might have stiff muscles or seizure-like movements. Don’t mistake this for a seizure - it’s still an overdose. If someone looks wrong and isn’t responding, assume it’s an overdose.
What to Do Immediately: The Three-Step Rescue
Time is everything. Brain damage starts after 4 to 6 minutes without oxygen. Here’s what you do - right now, no matter where you are:
- Call 911 - Don’t wait. Don’t text. Don’t call a friend first. Call emergency services immediately. Say: “Someone has overdosed on opioids. They’re not breathing.”
- Give naloxone - If you have it, use it. Naloxone (brand name Narcan) is a nasal spray that reverses opioid overdose in minutes. It’s safe. It won’t hurt someone who hasn’t taken opioids. If you’re unsure, give it anyway. Spray one dose into one nostril. Even if they don’t wake up right away, keep going.
- Stay with them - Don’t leave. Keep checking their breathing. If they stop breathing again, give another dose of naloxone. If they’re not breathing, start rescue breathing: tilt their head back, pinch their nose, give one breath every 5 seconds. Keep doing it until help arrives.
Some people worry about getting in trouble if they call 911. Most states have Good Samaritan laws that protect people who call for help during an overdose. Your priority is saving a life - not legal consequences.
How Naloxone Works - And Why It’s Not a Cure
Naloxone works by kicking opioids off the brain’s receptors. It’s like a reset button for breathing. It starts working in 2 to 5 minutes when sprayed in the nose. But here’s the catch: naloxone wears off in 30 to 90 minutes. Opioids like fentanyl can stay in the body much longer.
That means someone can wake up after naloxone - and then slip back into overdose when the naloxone wears off. This is why you must stay with them until paramedics arrive. You may need to give a second dose. Some people need three or more.
Naloxone is available without a prescription in 49 U.S. states. Many pharmacies sell it for $25 to $50 for a two-dose kit - down from $130 just a few years ago. Some community centers, clinics, and even libraries give it out for free. If you know someone who uses opioids, keep a kit in your car, your bag, or your home. It’s as important as a fire extinguisher.
What Happens After They Wake Up
Waking someone up with naloxone isn’t the end. It’s the beginning. They may be confused, scared, or angry. They might want to leave. Don’t let them.
Even if they seem fine, they need medical care. An overdose can cause pneumonia, lung damage, or brain injury from lack of oxygen. A doctor needs to check them out.
They also need help beyond the emergency room. Opioid use disorder is a medical condition - not a moral failure. Medications like methadone, buprenorphine, and naltrexone can help people recover. Counseling and peer support make a huge difference. Ask them to talk to a doctor about treatment options. Offer to go with them.

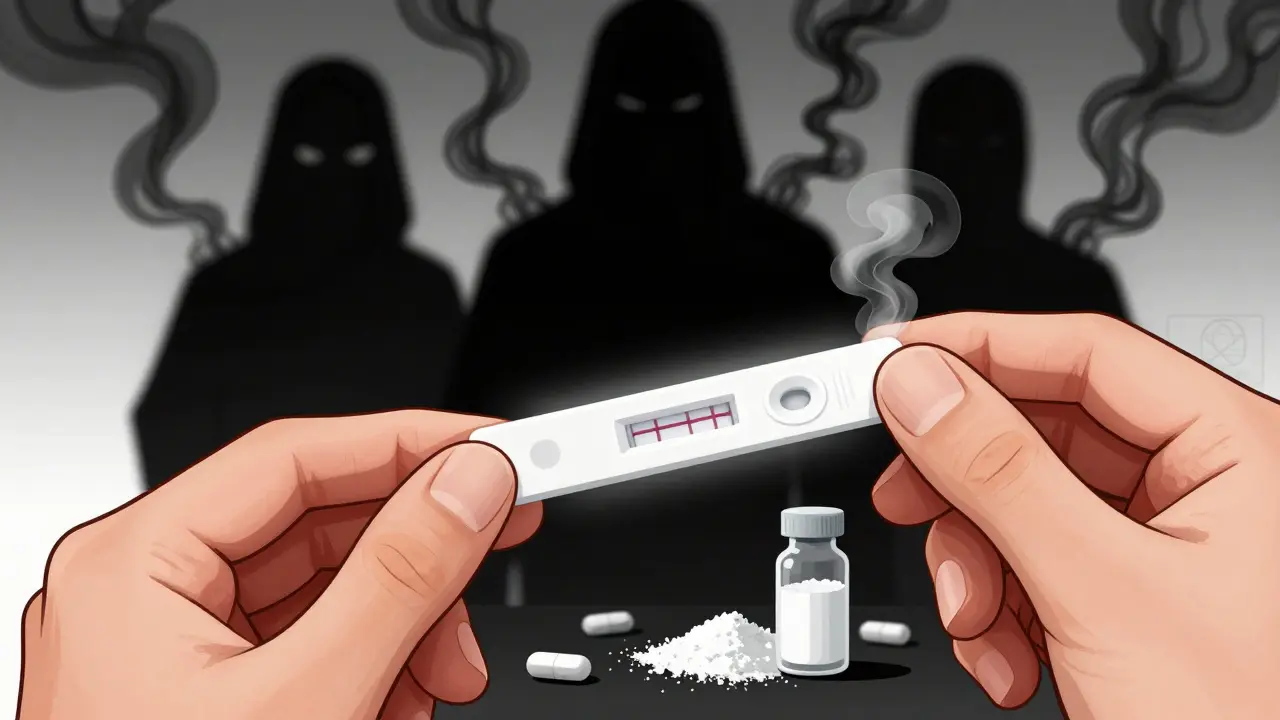
Prevention: Test Strips, Education, and Community
Many overdoses happen because people don’t know what’s in the drugs they’re taking. Fentanyl is often mixed into cocaine, Xanax, or counterfeit pills. It’s invisible. It’s odorless. It’s deadly.
Fentanyl test strips (FTS) are a simple, low-cost tool. You put a tiny bit of the drug in water, dip the strip, and wait a minute. If it shows a line, the drug contains fentanyl. It doesn’t stop someone from using - but it gives them a chance to use less, or not at all.
Communities that distribute naloxone and train people in overdose response have seen overdose death rates drop by up to 14%. That’s not magic. That’s action. Friends, family, neighbors - you - are the first line of defense.
Final Thought: You Can Be the Reason They Live
Opioid overdoses aren’t just statistics. They’re people - your neighbor, your cousin, your coworker. You don’t have to be brave. You just have to act.
Know the signs. Keep naloxone handy. Call 911. Stay until help comes. You don’t need permission. You don’t need to be perfect. You just need to care enough to do something.
Because in those first few minutes - when breathing stops and time runs out - you might be the only thing standing between someone and death.
Can naloxone harm someone who hasn’t taken opioids?
No. Naloxone only works on opioid receptors. If someone hasn’t taken opioids, it has no effect. It won’t cause harm, addiction, or side effects. If you’re unsure whether someone overdosed, give naloxone anyway. It’s safe.
What if I don’t have naloxone? Can I still help?
Yes. Call 911 immediately. Start rescue breathing - tilt their head back, pinch their nose, give one breath every 5 seconds. Keep doing it until help arrives. Rescue breathing keeps oxygen flowing to the brain. It can buy critical time. Never wait for naloxone if it’s not available.
Is naloxone only for heroin overdoses?
No. Naloxone reverses overdoses from any opioid - including prescription painkillers like oxycodone, fentanyl, morphine, codeine, and even synthetic opioids mixed into street drugs like cocaine or counterfeit pills. It works on all of them.
Can I give naloxone to a child or teenager?
Yes. Naloxone is safe for all ages, including children and teens. There’s no lower age limit. If a child or teen shows signs of opioid overdose, give naloxone and call 911 immediately. The dosage is the same as for adults - one spray in one nostril.
Where can I get naloxone for free?
Many pharmacies offer naloxone without a prescription. Some community health centers, harm reduction programs, and local health departments give it out for free. In Australia, naloxone is available over the counter at pharmacies. In the U.S., check with your local health department or visit websites like naloxone4all.org for free distribution sites near you.
Why do people keep overdosing even after being revived?
Naloxone wears off faster than most opioids - especially fentanyl. Someone might wake up, feel fine, and leave - only to slip back into overdose hours later. That’s why you must stay with them until paramedics arrive and they get checked at a hospital. Never assume one dose is enough.
Is it true that fentanyl is in most street drugs now?
Yes. The CDC and other health agencies confirm that fentanyl is now commonly mixed into cocaine, methamphetamine, counterfeit Xanax, and pills sold as oxycodone. People often don’t know they’re taking it. That’s why fentanyl test strips are a vital harm reduction tool - they help people avoid unknowingly taking a lethal dose.


Kristina Felixita
7 January / 2026OMG, I had no idea naloxone was this easy to use... I just got a kit for my purse after my cousin OD’d last year. Please, everyone, just keep one handy. It’s not a big deal, but it could save someone’s life. Seriously. Don’t wait.