SLT vs. ALT Laser Treatment Calculator
Select Your Treatment Preference
Choose between Selective Laser Trabeculoplasty (SLT) or Argon Laser Trabeculoplasty (ALT) to compare their features and outcomes.
Treatment Comparison Results
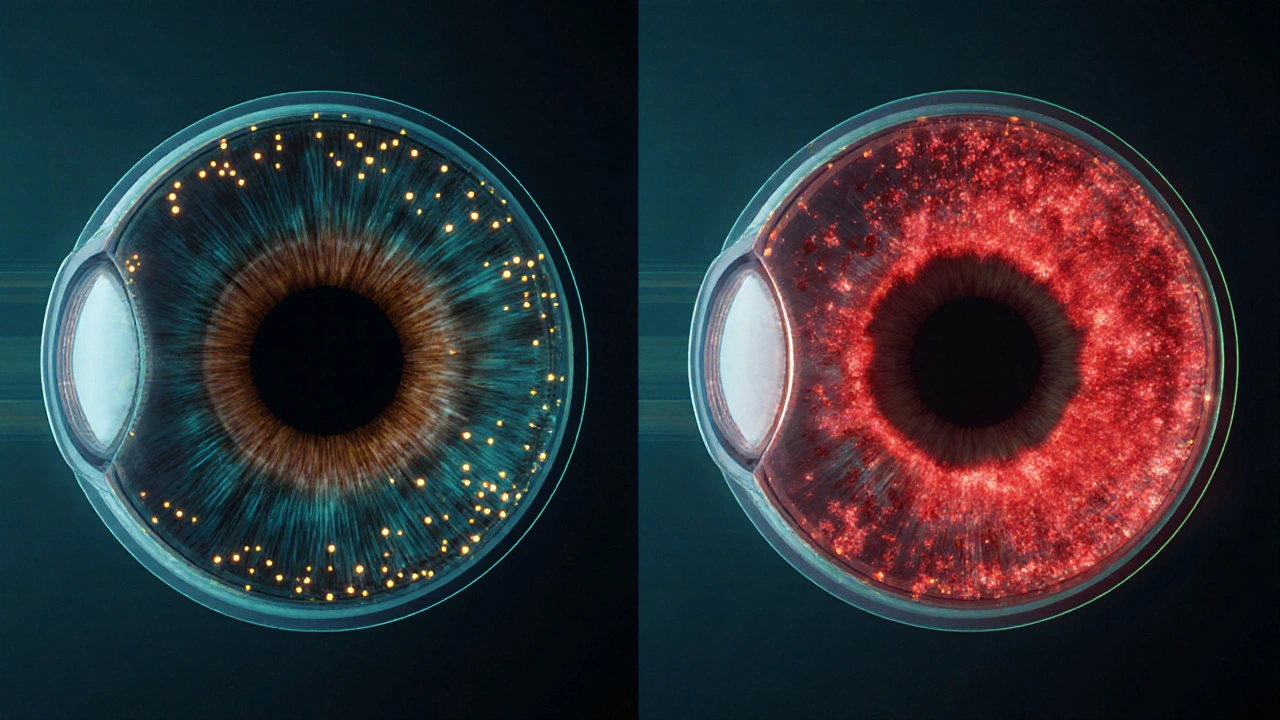
How Laser Treatment Helps Manage Eye Pressure
Laser therapies like SLT and ALT target the trabecular meshwork—the drainage system of the eye—to improve fluid outflow and reduce intraocular pressure (IOP).
- SLT uses low-energy pulses to activate cells without causing thermal damage, making it repeatable.
- ALT uses higher energy to create scarring, which improves drainage but limits re-treatment options.
Both treatments offer predictable IOP reductions and are generally safe with minimal side effects.
Key Takeaways
- Laser therapies such as Selective Laser Trabeculoplasty (SLT) and Argon Laser Trabeculoplasty (ALT) can safely lower intraocular pressure (IOP) without daily eye‑drop regimens.
- SLT works by targeting the trabecular meshwork with low‑energy pulses, offering repeatable treatment with minimal tissue damage.
- ALT uses higher‑energy argon lasers; it’s effective but may cause more inflammation, limiting repeat use.
- Candidates include patients with ocular hypertension, early‑stage glaucoma, or those who experience side‑effects from medications.
- Recovery is quick-most people resume normal activities within a day, but they should follow post‑procedure eye‑drop instructions to control inflammation.
When doctors discuss laser treatment is a non‑invasive procedure that uses focused light energy to modify eye tissue and lower intraocular pressure, they’re usually talking about ways to keep eye pressure from damaging the optic nerve. laser treatment eye pressure has moved from a niche option to a mainstream tool for managing ocular hypertension and early glaucoma, especially when patients can’t tolerate drops or want to avoid long‑term medication side‑effects.
Understanding High Eye Pressure
High eye pressure, technically called ocular hypertension is a condition where the intraocular pressure (IOP) exceeds the normal range (usually >21 mmHg) without obvious optic‑nerve damage. Over time, sustained pressure can compress the optic nerve fibers, leading to glaucoma-one of the leading causes of irreversible blindness worldwide.
Key risk factors include age over 40, family history of glaucoma, thin corneas, and certain ethnic backgrounds (e.g., African‑Australian descent). While eye drops are the first line of defense, up to 30% of patients struggle with adherence due to dosing complexity, cost, or local irritation.
Why Consider Laser?
Laser therapy offers several advantages over chronic medication use:
- Convenience: A single office visit can replace daily drops for months to years.
- Predictable IOP reduction: Clinical trials show an average 20‑30% drop in pressure after a successful SLT session.
- Safety profile: Minimal systemic side‑effects because the laser acts only on eye tissue.
- Cost‑effectiveness: Although the upfront procedure costs more, long‑term savings arise from fewer prescription refills and fewer doctor visits.
These benefits make laser a compelling option for people who:
- have medication intolerance or allergies,
- prefer a short‑term intervention over lifelong drops,
- need better IOP control before cataract surgery or other eye procedures.
Primary Laser Modalities
The two most common lasers for pressure control target the trabecular meshwork is a spongy tissue in the eye’s drainage angle that regulates aqueous humor outflow. By improving outflow, the pressure drops.
Selective Laser Trabeculoplasty (SLT)
SLT uses a frequency‑doubled Q‑switched Nd:YAG laser emitting 532‑nm light in short 3‑nanosecond pulses. The energy level is low enough to avoid thermal damage, so the procedure can be repeated if pressure rises again.
- Typical IOP reduction: 20‑30%. \n
- Duration of effect: 1‑3 years on average; repeatable.
- Side‑effects: Transient redness, mild inflammation, rarely a temporary spike in pressure.
Argon Laser Trabeculoplasty (ALT)
ALT predates SLT and uses a continuous‑wave argon laser (488nm/514nm) delivering higher energy burns to the meshwork. The induced scarring contracts the tissue, opening adjacent drainage channels.
- Typical IOP reduction: 20‑25%.
- Duration of effect: Often 2‑5 years, but repeat treatments are less common due to increased scarring risk.
- Side‑effects: More pronounced inflammation, higher chance of peripheral anterior synechiae (adhesions).
Laser Peripheral Iridotomy (LPI)
While LPI primarily treats angle‑closure glaucoma, it can indirectly lower pressure by creating a small hole in the peripheral iris, allowing aqueous humor to flow more freely.
Because LPI’s goal isn’t direct pressure reduction, we’ll focus the rest of the article on SLT and ALT, which are the mainstay for ocular hypertension management.
SLT vs. ALT: Quick Comparison
| Feature | Selective Laser Trabeculoplasty (SLT) | Argon Laser Trabeculoplasty (ALT) |
|---|---|---|
| Laser type | Q‑switched Nd:YAG (532nm) | Continuous‑wave Argon (488/514nm) |
| Energy per pulse | Low (0.3‑1.2mJ) | Higher (50‑100mJ) |
| Mechanism | Cellular activation without thermal damage | Thermal coagulation and scarring |
| Typical IOP drop | 20‑30% | 20‑25% |
| Repeatability | Yes, up to 3‑4 times | Limited, high scarring risk |
| Typical side‑effects | Transient redness, mild inflammation | More inflammation, possible synechiae |
| Procedure time | 5‑10 minutes | 10‑15 minutes |
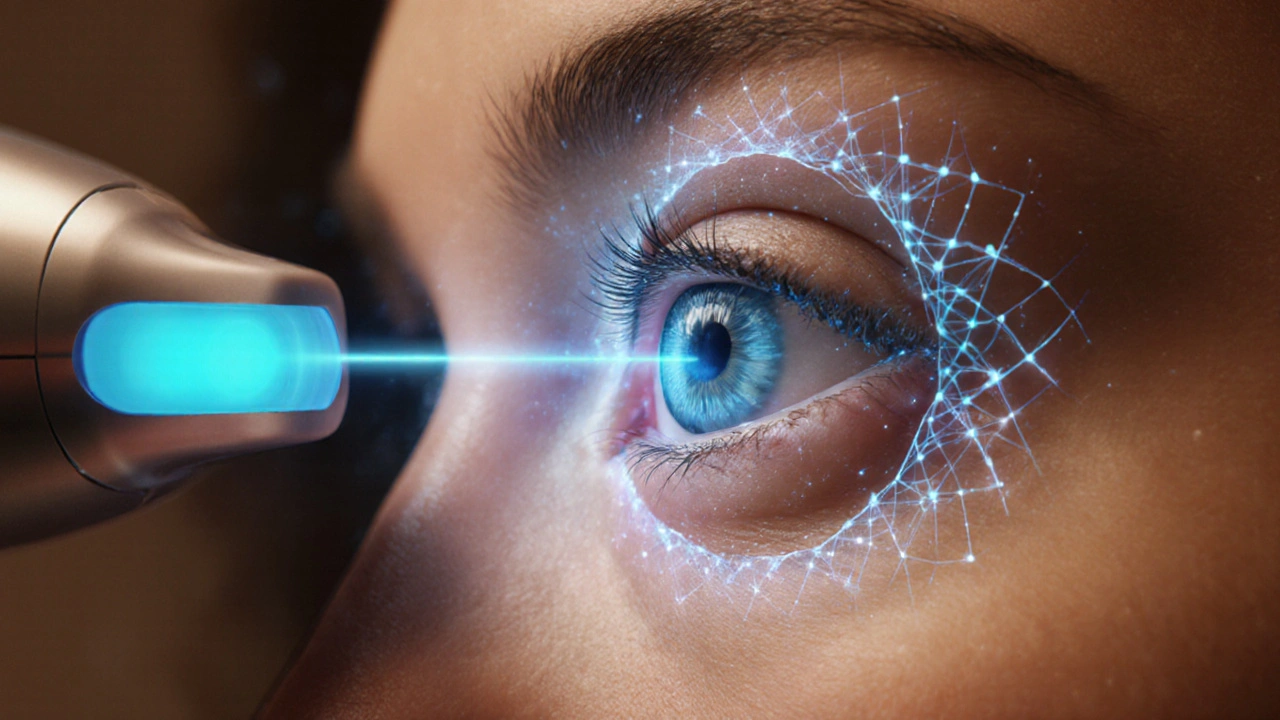
What Happens During a Laser Procedure?
- Pre‑procedure assessment: The ophthalmologist is a medical doctor specialized in eye diseases who evaluates the angle, IOP, and overall eye health checks the drainage angle with gonioscopy.
- Topical anesthesia: One or two drops numb the surface-no injections needed.
- Patient positioning: You sit upright, looking into a slit‑lamp microscope that also houses the laser.
- Laser delivery: The doctor fires short pulses over 180‑360 degrees of the trabecular meshwork. You’ll feel brief flashes but no pain.
- Post‑laser medication: Usually a short course of steroid or non‑steroidal anti‑inflammatory drops for 3‑5 days to control swelling.
- IOP check: The doctor measures pressure 1 hour later and again the next day to ensure there’s no spike.
The whole visit typically lasts less than 30 minutes, and you can drive home afterward.
Who Can Benefit?
Ideal candidates share one or more of the following:
- Diagnosed with ocular hypertension (IOP >21mmHg) but no significant optic‑nerve damage.
- Early‑stage primary open‑angle glaucoma where medication adherence is poor.
- Patients on multiple drops who experience ocular surface disease.
- Those scheduled for cataract surgery who need better pressure control beforehand.
Contra‑indications include clogged drainage angles (angle‑closure), active eye infection, or severe corneal disease that would interfere with laser delivery.
Risks, Side‑effects, and Aftercare
Laser trabeculoplasty is considered safe, but no medical procedure is risk‑free.
| Side‑effect | Incidence | Typical Management |
|---|---|---|
| Transient redness | 70‑80% | Artificial tears, avoid rubbing |
| mild inflammation | 30‑40% | Short‑course steroid or NSAID drops |
| IOP spike (10‑15mmHg) | 5‑10% | Additional drop of carbonic‑anhydrase inhibitor; monitor closely |
| Rare peripheral anterior synechiae | <1% | Prompt treatment with peripheral iridotomy if needed |
Most patients feel normal within a day. It’s still wise to avoid swimming or hot tubs for 24 hours, and to keep the prescribed anti‑inflamatory drops as directed.
Laser vs. Medication: Making the Choice
Both options effectively lower IOP, but they serve different lifestyles.
- Adherence: Laser eliminates daily dosing; great for busy or forgetful patients.
- Cost over time: While the laser fee (AU$1,200‑1,500) is upfront, the cumulative cost of drops (AU$30‑50/month) adds up.
- Adjustability: Medications can be tweaked daily; laser effect is fixed until the next treatment.
- Side‑effect profile: Drops may cause allergic reactions, systemic absorption; laser side‑effects are short‑term and ocular.
In practice, many eye doctors start with drops, then propose laser if pressure goals aren’t met or if adherence wanes. Some patients even combine a low‑dose drop regimen with laser for maximal control.
Future Directions
Research in 2024‑2025 is exploring micropulse laser technology that delivers ultra‑short bursts, potentially reducing inflammation even further. Early trials suggest comparable IOP drops with virtually no post‑procedure redness. While still awaiting widespread approval, the trend points to even safer, repeatable laser options.
Frequently Asked Questions
How long does the IOP‑lowering effect of SLT last?
On average, SLT keeps pressure down for 2‑3 years, but many patients see benefits up to 5 years. Because the procedure causes minimal tissue damage, it can be safely repeated if pressure climbs again.
Is the laser painful?
You’ll feel brief flashes of light, but the topical anesthetic makes the process virtually painless. Most people describe it as a quick, gentle tingling.
Can I have laser treatment if I’m already using eye drops?
Absolutely. In many cases the laser is performed while you continue your drops, and the doctor may taper the medication afterward based on your new IOP readings.
What should I avoid after the procedure?
Avoid rubbing your eye, swimming, or hot tubs for at least 24hours. Keep using the anti‑inflammatory drops as prescribed and attend the follow‑up IOP check.
Is laser treatment covered by Australian Medicare?
Medicare typically subsidises the procedure when it’s medically necessary, but coverage details vary by state and clinician. It’s best to check with your eye clinic’s billing department.



Karen Gizelle
8 October / 2025Honestly, the medical community should stop treating eye pressure like a DIY project.
When doctors push laser treatement without stressing the lifelong commitment to follow‑up, they’re flirting with negligence.
Patients deserve a clear roadmap, not a vague promise that “pressure will drop.”
Even a tiny typo in consent forms can cause real misunderstanding.
We must hold ourselves to a higher standard, otherwise we’re just playing with people’s sight.