MS Exercise Intensity Calculator
Calculate your safe exercise intensity based on heart rate and RPE (Rate of Perceived Exertion) guidelines for multiple sclerosis patients.
1=Complete rest, 10=Maximum exertion. Aim for RPE 3-4 for MS patients.
Enter your information to see safe exercise intensity recommendations
Quick Summary
- Regular exercise benefits for sclerosis patients can slow disease progression and boost quality of life.
- Aerobic, strength, flexibility, and balance activities each target specific MS symptoms.
- Start with low‑intensity sessions, monitor heat sensitivity, and progress gradually.
- Working with a physiotherapist ensures safety and personalized programming.
- Track workouts, set realistic goals, and stay connected to support groups for lasting motivation.
When it comes to managing sclerosis, Exercise is a physical activity that improves muscle strength, cardiovascular health, and nervous system function. For people living with multiple sclerosis (MS), staying active isn’t just a lifestyle choice-it’s a therapeutic tool that can mitigate fatigue, preserve mobility, and even support cognitive health. This guide walks you through the science, the safe‑start steps, and practical tips to turn workout time into a real health boost.
Why Exercise Matters for Sclerosis
Multiple Sclerosis is a chronic autoimmune disease that attacks the myelin sheath around nerve fibers, causing unpredictable bouts of weakness, numbness, and fatigue. While medication tackles the immune attack, exercise targets the downstream effects-muscle atrophy, cardiovascular deconditioning, and mood disturbances. Studies from 2023-2024 show that participants who engaged in moderate‑intensity aerobic activity at least three times a week experienced a 0.5‑point slower rise in the Expanded Disability Status Scale (EDSS) compared with sedentary peers.
Beyond numbers, patients report better sleep, sharper focus, and a stronger sense of control over their bodies. These subjective gains are crucial because MS often brings feelings of helplessness; a regular workout routine can re‑anchor confidence.
How Exercise Impacts Core Symptoms
- Mobility and Strength: Resistance training stimulates muscle protein synthesis, counteracting the weakness that MS can cause in the legs and arms.
- Fatigue Management: Paradoxically, low‑to‑moderate cardio improves mitochondrial efficiency, reducing the daytime slump many patients face.
- Mood and Depression: Endorphin release from aerobic sessions lifts mood, cutting the risk of clinical depression by up to 30% in longitudinal studies.
- Cognitive Function: Regular aerobic exercise supports neuroplasticity, helping preserve memory and processing speed.
- Spasticity and Balance: Stretching and balance drills improve joint range of motion, easing muscle stiffness and lowering fall risk.
Safe Exercise Guidelines for Sclerosis Patients
Before lacing up shoes, get a baseline assessment from a qualified physiotherapist. They’ll check heart rate response, heat tolerance, and current mobility limits. Here’s a simple rule‑of‑thumb framework:
- Start Low, Go Slow: Begin with 10‑minute sessions at 40-50% of maximum heart rate (MHR). Use the “talk test”-you should be able to speak in full sentences.
- Frequency: 3‑4 days per week, alternating cardio and strength days to allow recovery.
- Intensity: Aim for a Rate of Perceived Exertion (RPE) of 3-4 on a 0‑10 scale. Increase by 5‑10% every two weeks if you feel comfortable.
- Heat Sensitivity: MS patients often worsen in temperatures above 86°F (30°C). Choose climate‑controlled gyms, swim in cool water, or schedule outdoor walks during early morning/evening.
- Hydration & Stretching: Keep a water bottle handy and end each session with 5‑10 minutes of gentle stretching.
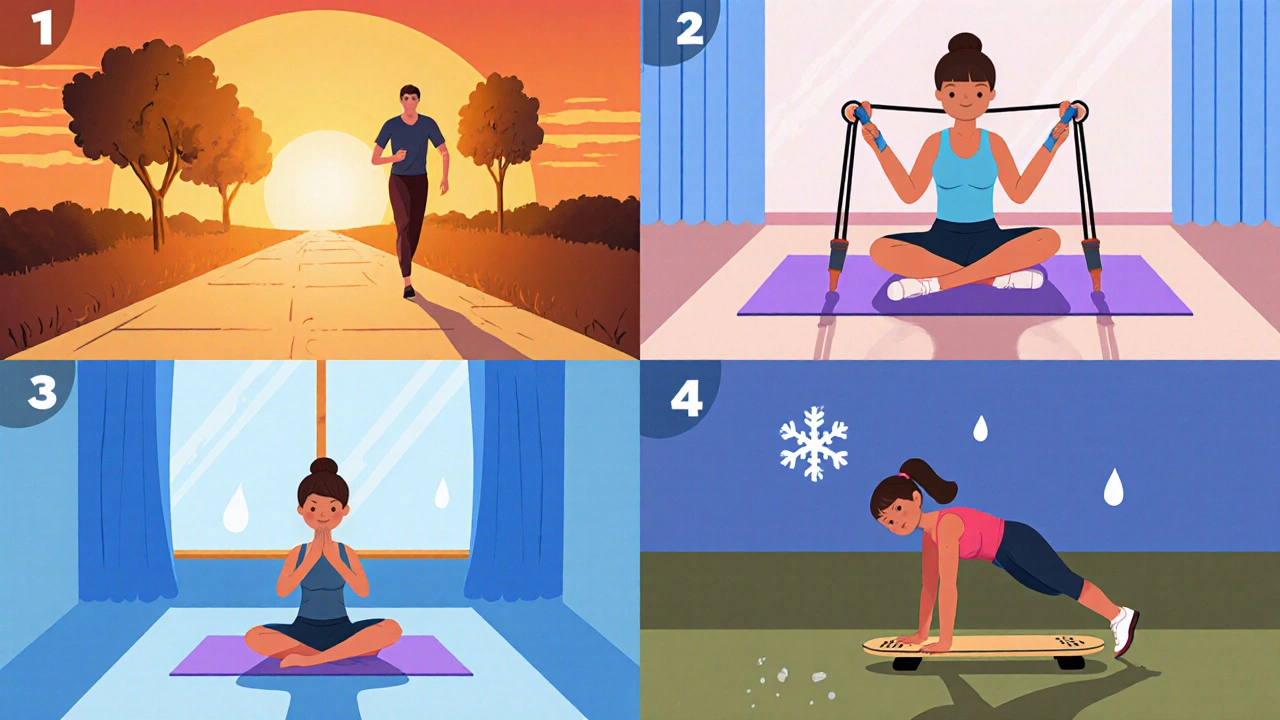
Choosing the Right Activity
Different exercise modes address distinct symptoms. The table below compares four core categories and offers quick recommendations.
| Type | Primary Benefit | Suggested Frequency | Intensity Guideline |
|---|---|---|---|
| Cardiovascular (e.g., brisk walking, stationary bike) | Improves endurance, reduces fatigue | 3-4 times/week | 40-60% MHR, RPE 3-4 |
| Strength Training (machines, resistance bands) | Builds muscle mass, combats weakness | 2-3 times/week | 8-12 RM, RPE 4-5 |
| Flexibility (Yoga, static stretching) | Reduces spasticity, enhances range of motion | Daily or post‑workout | Hold each stretch 20-30 sec, no pain |
| Balance & Proprioception (Tai chi, balance board) | Lowers fall risk, improves coordination | 2-3 times/week | Focus on controlled movements, RPE 2-3 |
Building a Personal Routine
Start with a week‑long template and adjust based on how you feel. Below is a sample schedule for a beginner with mild mobility issues:
- Monday - Cardio: 15‑minute stationary bike at RPE 3, followed by 5‑minute gentle stretch.
- Tuesday - Strength: Upper‑body resistance bands (2 sets of 10 reps for each major muscle), finish with shoulder rolls.
- Wednesday - Rest or Light Yoga: 10‑minute seated yoga sequence focusing on breathing.
- Thursday - Cardio: 20‑minute brisk walk outdoors before 8 am (cool temperature).
- Friday - Balance: Tai chi video (15 min) plus ankle circles.
- Saturday - Combined: 10‑minute bike + 10‑minute resistance band circuit.
- Sunday - Rest: Recovery, hydrate, review weekly log.
Log each session’s duration, RPE, and any symptoms (e.g., increased fatigue or heat intolerance). After two weeks, aim to add 5 minutes to cardio or an extra set to strength exercises.

Common Pitfalls and How to Avoid Them
- Overexertion: Jumping from 10‑minute walks to 45‑minute runs triggers relapse‑like fatigue. Stick to the 10% rule-don’t increase volume by more than 10% per week.
- Ignoring Heat Sensitivity: If you feel sudden weakness, stop, cool down, and hydrate. Consider cooling vests for indoor cycling.
- Lack of Variety: Repeating the same motion can lead to joint strain. Rotate cardio, strength, and flexibility every other day.
- Skipping Professional Guidance: A physiotherapist can tweak form, suggest adaptive equipment, and spot early signs of overuse.
Tracking Progress and Staying Motivated
Visual feedback drives adherence. Use a simple spreadsheet or a free app like MyFitnessPal to note:
- Date and type of activity
- Duration and intensity (RPE)
- Subjective symptom score (0‑10)
Review the log monthly; look for trends such as reduced fatigue scores or improved walking distance. Celebrate milestones-whether it’s a 5‑minute longer bike ride or an extra set of squats.
Joining an MS‑focused exercise group, either online or at a local community center, adds accountability and shared experience. Many national MS societies run free virtual classes that cater to varying ability levels.
Final Thoughts
Exercise isn’t a cure, but it’s a powerful adjunct that can reshape the daily reality of sclerosis patients. By starting low, listening to your body, and building a balanced routine, you harness the body’s own resilience to fight fatigue, preserve mobility, and lift mood. Pair these habits with regular medical care, and you’ll give yourself the best shot at a fuller, more active life.
How often should someone with MS exercise?
Current guidelines suggest 3‑4 sessions per week, mixing aerobic, strength, flexibility, and balance work. Start with short, low‑intensity bouts and increase duration by no more than 10% each week.
Is it safe to exercise on a day when MS symptoms flare?
If you’re experiencing a significant relapse (new weakness, vision loss, or severe fatigue), it’s best to pause intense activity and consult your neurologist. Light stretching or gentle mobility work may still be okay, but listen to your body.
What equipment is most useful for home workouts?
A set of resistance bands, a sturdy chair for support, a yoga mat, and a stationary bike or elliptical (if space permits) cover most needs. Add a balance pad or wobble board for proprioception drills.
Can swimming help with spasticity?
Yes. The cool water reduces temperature‑triggered spasticity, while gentle resistance improves muscle tone without stressing joints. Aim for 20‑minute laps at a comfortable pace.
How do I know if I’m overdoing it?
Warning signs include lingering soreness beyond 48 hours, worsening fatigue the next day, or heat‑induced worsening of symptoms. If any of these appear, cut back intensity and discuss adjustments with a physiotherapist.



cariletta jones
22 October / 2025Exercise can be a game‑changer for folks with MS. Start small, stay consistent, and celebrate each win.